25 Questions for Kidney Transplant
As the transplant world convenes for WTC, these are the questions on my mind about where we are—and where we’re headed.
As the World Transplant Congress kicks off here in San Francisco, we find ourselves at a crossroads. On the one hand, the science and medicine of kidney transplantation (KT) has reached new heights. In the past twelve months, we’ve witnessed landmark achievements in gene editing, perfusion, xenotransplant, and clinical trials. On the other, I think it’s fair to say that wave of optimism has been met with equal and opposite force by several waves of scrutiny and calls for accountability at every level, from donor families to the highest branches of government.
While hope is warranted, public trust is under pressure, and the system we have now may not look like the system we have a year from now. We continue to see and hear of inefficiencies that persist across referral, evaluation, donation, and allocation. As talk of innovation resonates through the airwaves (including on this platform), I’m reminded that every single one of these new tools and treatments depends on a functioning system within which to operate.
So, as I lace up my walking shoes for the next few days of scientific sessions, research posters, industry presentations, and serendipitous meetings, I thought I’d share a few questions on my mind.
Please know this list is incomplete. It’s my personal attempt to weave imagination with uncertainty, and hope with caution. If you’re reading this, whether you’re attending this event or not, you are an important part of this dialogue, and I’d love to hear what you think. Are these the right questions to be asking? What else should we be asking?
What’s inside:
Donation, Access & Capacity
Governance, Technology & Transparency
Science, R&D, and Organ Innovation
Immunosuppression, Cancer & LT Outcomes
Payment Models & System Incentives
Donation, Access & Capacity
The kidney transplant waitlist is growing again—for the first time in years. As more patients enter an already strained system, we explore the forces driving that growth, the implications for wait times, and the operational friction in the referral-to-listing pipeline. These questions explore how we can better support inactive patients, improve outcomes for highly sensitized individuals, and design a more equitable and efficient approach to waitlist management and organ matching.

1. Every eight minutes, someone gets added to the transplant waitlist. That’s 180 people a day. For those listed today, will the system look much different by the time they get a kidney? And will we be adding more or fewer people each day by then?
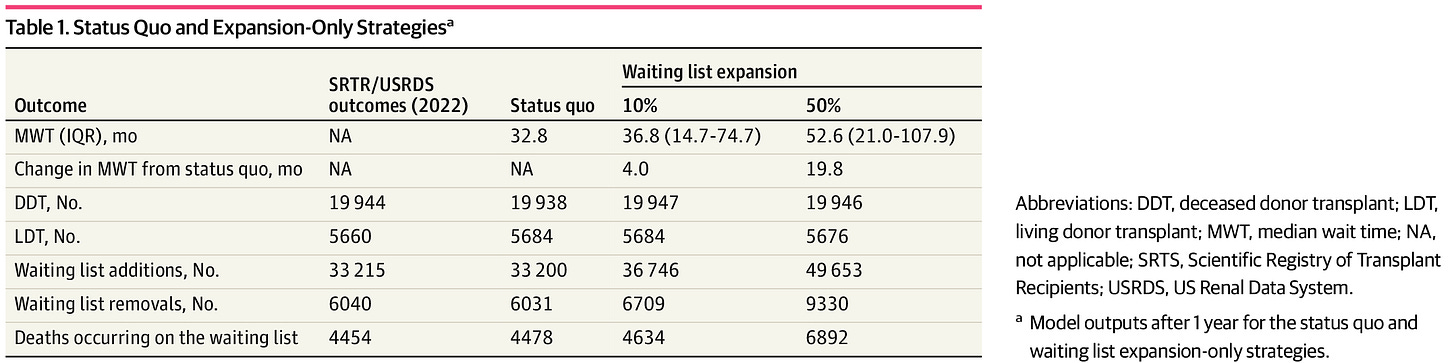
2. The waitlist had been shrinking for years. Last year that trend reversed course. What’s driving it (see chart above)? And what does it signal about our national transplant capacity and expectations for patients going forward?
3. How will a larger waiting list affect wait times? As the number of people waiting continues to increase faster than increases in volumes, we should expect wait times to increase. But by how much, and what can we do at the program or patient level to address it?
A recent study showed adding 10% or 50% more patients to the waiting list was estimated to lengthen wait times by 4 to 20 months.
4. How do we streamline the referral, evaluation, and waitlisting (REW) process?
From referral to activation, the current system is opaque and full of friction—especially for marginalized communities. A 2024 paper by Drs. Hippen, Hart, and Maddux proposes a triage model prioritizing patients likely to be transplanted soonest, freeing up resources for those most likely to benefit.
5. How do we support the nearly half of the 90,000 people waiting on a kidney who are considered inactive? That means a patient is ineligible for transplant if a kidney becomes available due to medical, psychosocial, financial, or administrative factors. Since a 2003 amendment by OPTN, the number of patients designated as inactive has risen ~5x. Patients on the inactive waitlist for KT have an elevated risk of waitlist mortality, longer wait times, and lower odds of getting a transplant.
6. What about patients with high panel reactive antibodies (PRA), who still face far lower access to transplant? Highly sensitized patients face a unique challenge. What new strategies—from desensitization to policy levers—are being developed to help address this gap? Unintended consequences of the 2014 changes to the kidney allocation system algorithm for highly sensitized patients provide clear examples of why policy change is necessary, hard, and iterative.
7. Why hasn’t living donation grown in more than two decades? Despite reforms and rising transplant demand, living donation hasn’t grown much in twenty years. We wrote about this one in our recent piece ‘5 Charts That Explain Kidney Care’. Even with new policies aimed at removing financial and logistical barriers, the living donor total has never surpassed 6,900 in a single year. Many point to needed protections for donors as a top priority. Fortunately, there’s movement on that front in Washington.
8. Is paired donation still growing? Yes, kidney paired donation (KPD) is increasing. A recent study showed 1 in 5 living donor kidney transplants (LDKTs) was facilitated by KPD in 2021. That said, 40% of the programs reported not performing any KPD transplants that year. The same paper highlights the need for understanding barriers to pursuing and expanding KPD at the center level and the need for more detailed and accurate data collection at the national level.
Governance, Technology & Transparency
As the transplant system evolves, so do the questions of who’s responsible for its results—and what it will take to modernize. In this section, we explore the mechanics of oversight, the limits of current reform efforts, and what’s needed to rebuild public trust. From federal accountability and fragmented governance to digital infrastructure and stakeholder inclusion, we ask: Is the system keeping up with the moment?
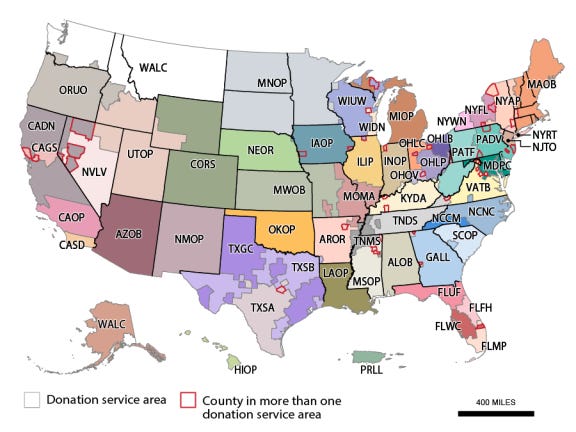
9. Reform is underway. Are policy and legislative levers moving us in the right direction? In the case of organ procurement organizations (OPOs), you might recall the 2020 Conditions for Coverage Final Rule, which set 2026 as the enforcement date for new performance measures. That’s now just around the corner. For context, each of the 56 OPOs is designated to a donor service area (DSA) under a 4-year exclusive agreement, tied to their recertification cycle. As CMS continues shaping its OPO strategy, the question remains: Can reform move as fast (or faster) than the problems it was designed to fix?
10. Can we restore public trust in donation after recent headlines? Allegations of misconduct and harm during organ recovery have shaken confidence (here, here, and here). People in and outside the kidney community have expressed alarm. As a friend of mine often says, “Organ transplant is a miracle—and it has real problems.” Both can be true. The challenge is protecting the miracle by confronting the problems head-on.
11. What role are patients playing in redesigning governance structures? Stakeholder mapping efforts show overlapping influence across payers, providers, vendors, and advocates. A recent shakeup of patient and donor representatives from the OPTN board of directors left a lot of people with questions. You can find the current board and their personal statements here.
12. Is the transplant system ready to invest in the tech and talent needed for modernization? From call centers and paper manifests to machine learning and real-time logistics, the contrast is staggering. So what’s stopping digital transformation? Is it cost? System inertia? Misaligned incentives? A deeper reluctance to change? Or something else altogether?
13. Why is it still so hard to extract useful data from a patient’s referral through to activation? Despite EMR integrations and built-in tools, most transplant evaluation data remains highly manual and fragmented. Some centers rely on full-time coordinators or even surgeons combing through spreadsheets for hours each day. Patients at major centers may hear nothing between getting listed and getting the call. There has to be better ways to enable transplant center teams to keep patients engaged, active, and ready for transplant— right?
14. What is it about transplant specifically that prevents a real-time, nationwide transplant logistics database? Legacy tech is still blamed for lost organs and missed matches. Why haven’t we built a platform with modern tools—blockchain for tracking, AI for matching, even chatbots for patient experience? Pick a buzzword—we’re overdue for progress. And if you’re building any of these tool, I’d love to hear from you.
Science, R&D, and Organ Innovation
Breakthroughs in organ preservation, immune tolerance, and xenotransplantation are reshaping the future of kidney care. But questions remain about safety, ethics, and how far off routine application really is.
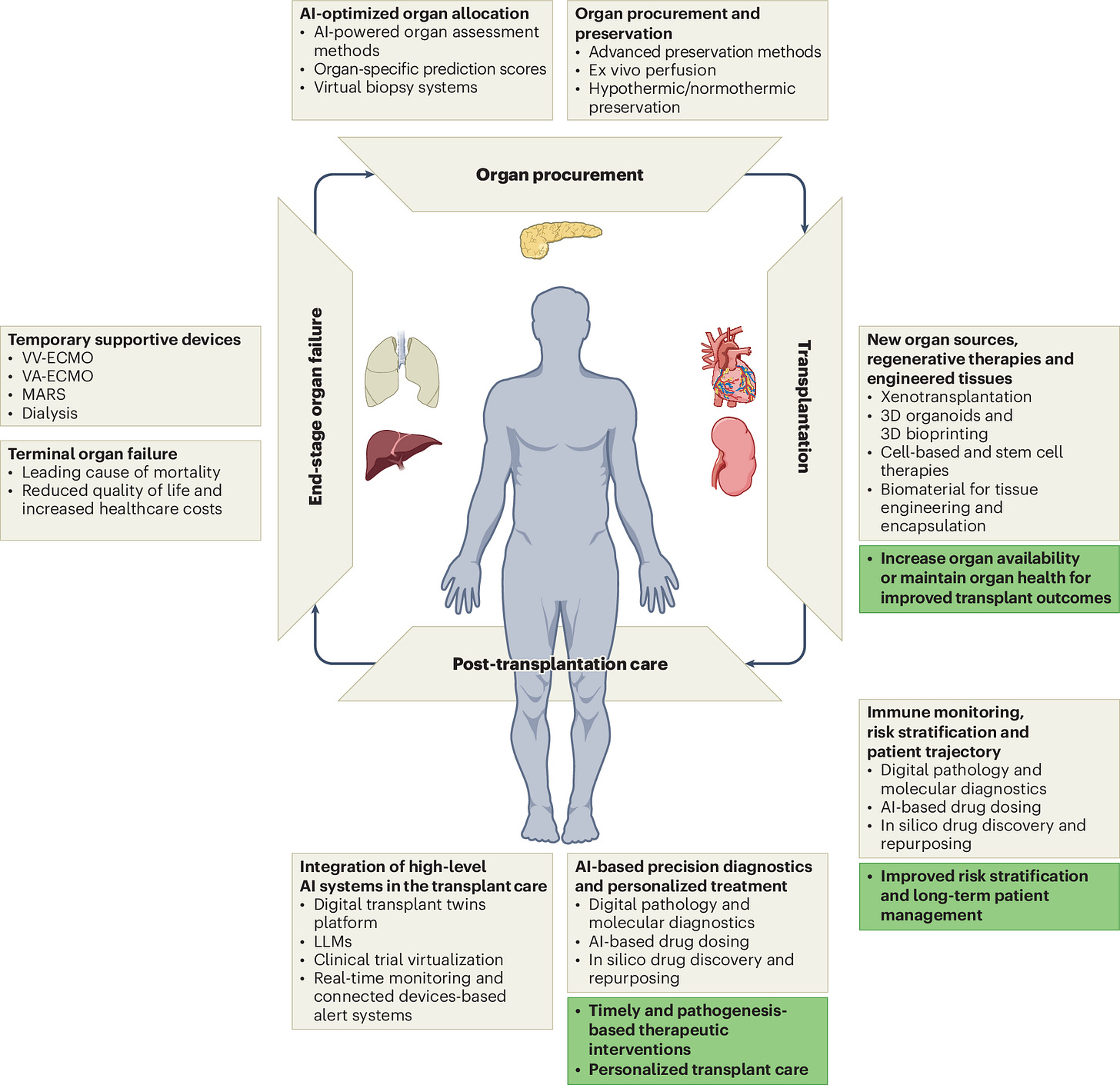
15. What will it take for pig kidneys to become a routine option—not just a last resort? Trials are underway, but immune rejection, physiologic mismatch, and durability remain big challenges. Which hurdles are most urgent—and most solvable?
16. How should programs prepare for accepting higher-KDPI kidneys—and how do we support that shift? Low utilization persists even when outcomes could be acceptable. I was curious about what goes into such a complex, time-sensitive decision making process. This recent study quantified the variability in kidney offer acceptance decisions attributable to clinicians vs centers and examined the role of donor quality in acceptance decisions.
17. What do kidney patients actually think about xenotransplantation?
Trials are underway—I’d like to know how patients perceive the risks, ethics, and tradeoffs of genetically modified pig organs. When thinking about all available treatment options, how does xeno stack up? In 2023 the NKF hosted a patient focused drug development meeting on this topic and produced this Voice of the Patient report. I’d love to see more of this as we navigate the next chapter in xeno.
Immunosuppression, Cancer & LT Outcomes
As research advances toward immune tolerance, long-term transplant survivorship is becoming its own clinical frontier.
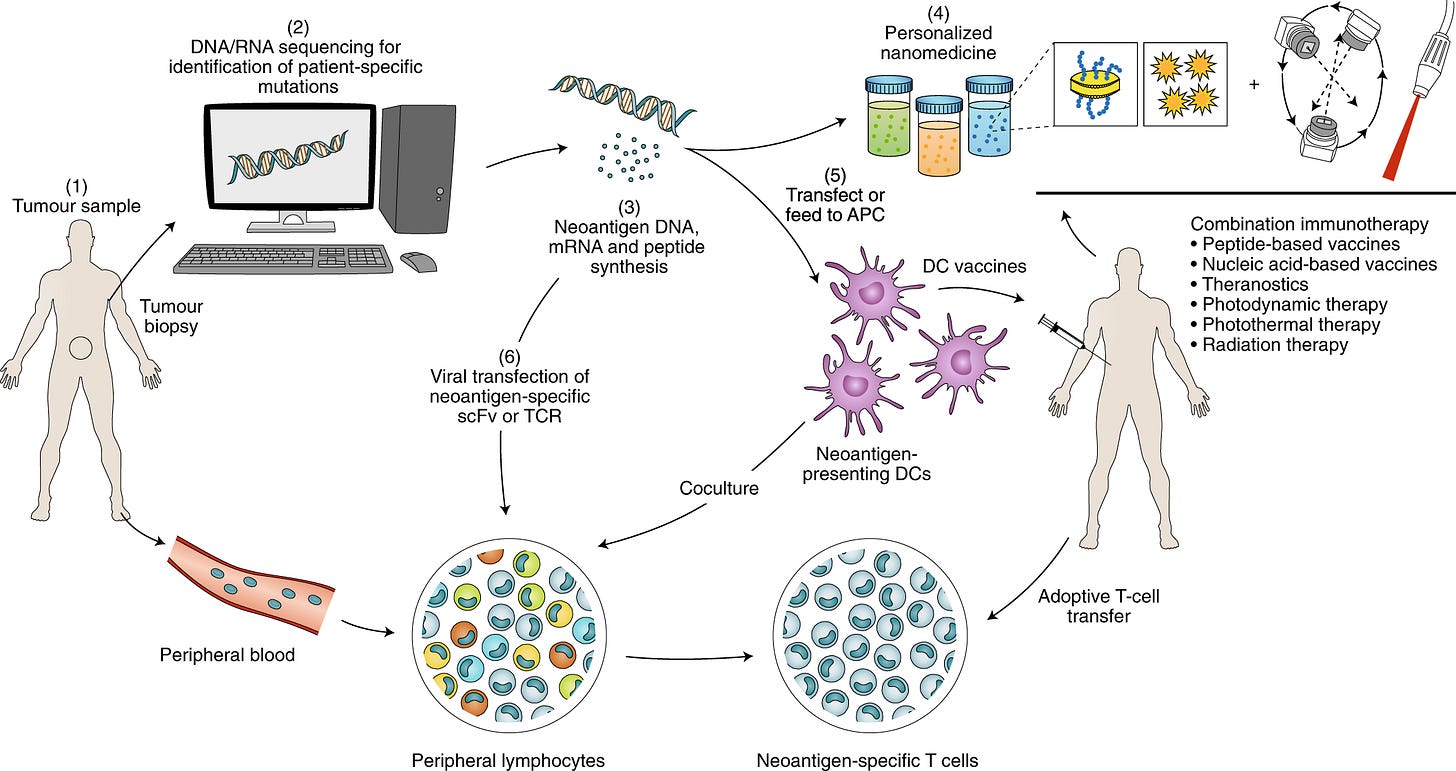
18. Is a post-transplant life without lifelong immunosuppression finally within reach? Results from a recent phase 3 clinical trial show what was once considered impossible: safe discontinuation of immunosuppressive medications after kidney transplant. In the study, recipients who received both a kidney and stem cells from a closely matched sibling were weaned off all immunosuppression within a year—75% remained off meds for over two years. I will say, immune checkpoint inhibitors in transplant is a fascinating space.
19. How do we better monitor and manage cancer risk in long-term transplant recipients? We know solid organ transplant recipients (SOTRs) are at increased risk of developing and dying from cancer. This review looked at the availability, quality and consistency of cancer screening recommendations in clinical practice guidelines (CPGs). Dr. Joe Scalea and the team at MUSC built a tool that weeks worth of chart review in seconds to help identify and stratify levels of risk post-transplant.
“Based on our estimates, about 700,000 data points per year need to be evaluated just to manage our kidney transplant group of post-op patients.”
20. Are we missing opportunities to individualize immunosuppression using real-world data? With hundreds of thousands of transplant recipients across the U.S., why haven’t we built adaptive, personalized post-transplant regimens? I know, I make it sound far simpler than it is. This 2019 paper describes a few possible engineering approaches, including the design of biomaterials, delivery strategies and nanotechnology solutions. Which do you think comes first, n-of-1 immuno-suppression, or eliminating the need for them altogether?
Payment Models & System Incentives
Follow the money: as a whole the transplant system still rewards volume over value, and dialysis over transplant. Until that changes, transformation will be limited. Fortunately, kidneys remain at the forefront of payment model innovation.
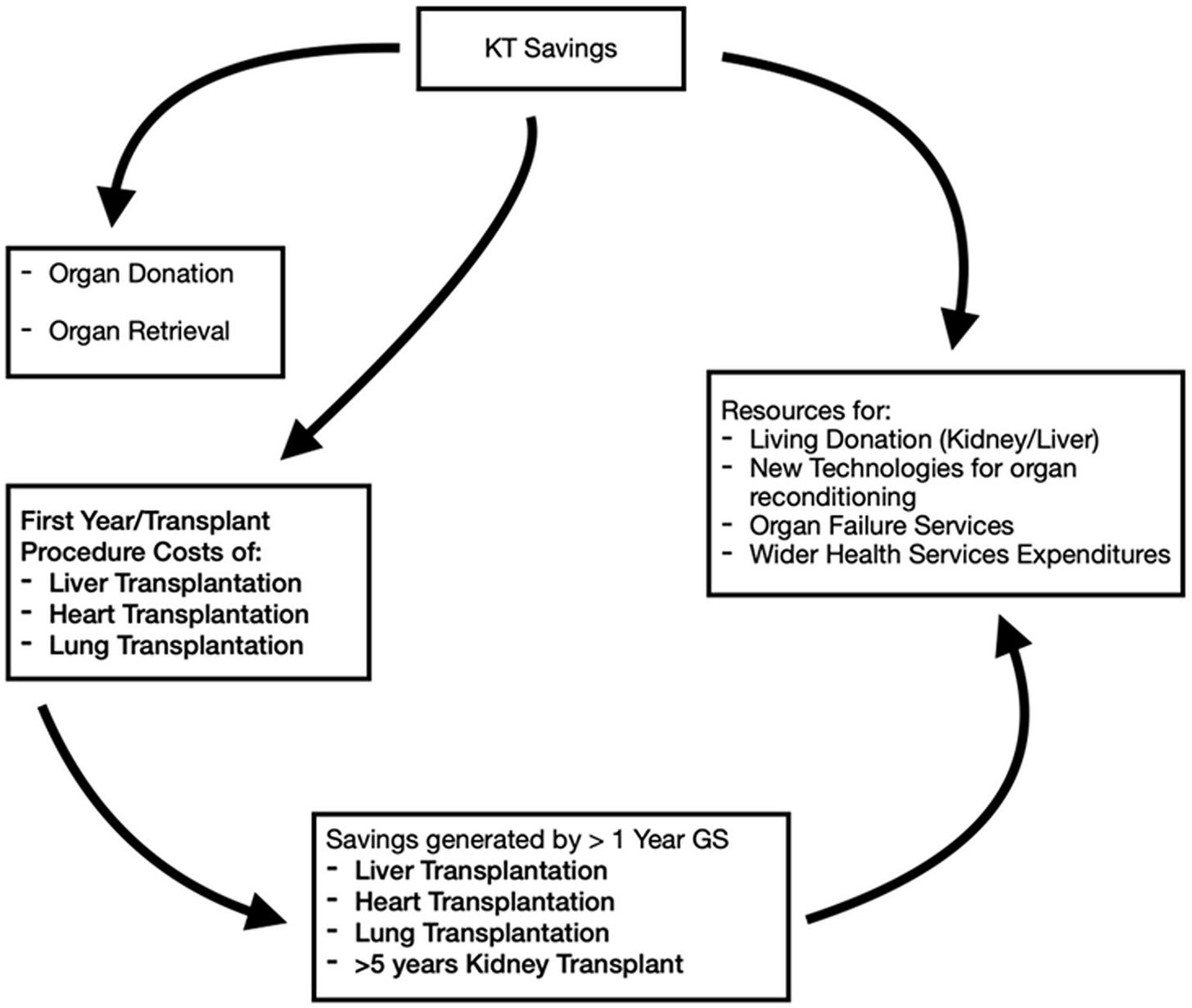
21. Will the IOTA model improve organ acceptance—and will we see volumes increase by other means? Candidly, I’ve heard mixed feelings on this one. Many say the model’s incentives are more carrot than stick. One thing is for sure: if we’re asking centers to take more risks (see KDPI above), the math needs to math.
22. Will we see an impact in listings after the Kidney Transplant Bonus (KTB) departs the KCC model? Will referring practices deprioritize transplant in response, or find new ways to maintain momentum from new workflows and practices?
23. Can we design bundled payments that truly reward long-term outcomes—not just surgical throughput? Dialysis bundles reshaped that sector—for better and worse. Could a similar approach help transplant patients, programs, and payers?
24. How are transplant service lines viewed inside health systems? I find that many programs are often high-profile but under-resourced. Can centers grow volumes without proportional investment? What is expected— financially, operationally, or clinically—of programs that are seeking to grow their volumes by 25%, 50%, even 100%+ over the next 3-5 years?
25. Is there a path to ethically compensating donors or donor families for their contribution? Last August I wrote about the End Kidney Deaths Act, which outlines a ten-year pilot program offering a $10,000 refundable tax credit per year for five years (totaling $50,000) to non-directed living kidney donors who donate to a stranger at the top of the waitlist. I’m hoping to get an update on where things stand in the current Congress. One notable example where this has worked? Iran.
What do you think?
Are you working on one of these questions—or wrestling with another one we missed? Whether you’re at WTC this week or watching from afar, you are part of this conversation and I’d love to hear from you. Hit reply or reach out.
We’ll be publishing a WTC follow-up spotlighting the people, projects, and policies aiming to answer a few of these questions (and a few I didn’t ask). Thanks for being here and supporting this work.
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)

This is such a great summary! Much promise and some big, important challenges too. I hope sunlight will catalyze ever more transparency and that those together will light the way forward.