Signals Recap: A Week of Firsts — Kidney Disease Goes Global, Personalized CRISPR, MAHA's Report, CMS Targets MA, & more
Your biweekly collection of news, research, funding & community voices shaping the future of global kidney health

It’s been a busy few weeks, and I’m just back from Washington, DC, where I had the chance to join an incredible group of peers at the 2025 Kidney Innovation Conference. This year’s theme—Innovation through Collaboration—set the tone for two days of listening, learning, and leaning in. From workshops on pediatric trials and APOL1 roadmaps to patient stories and a powerful keynote from Dr. Robert Montgomery, it left me energized about what’s possible. I’ll be putting together a series of posts on ideas that bubbled to the surface and the people behind them, so stay tuned. It was also a week of firsts: the World Health Assembly passed the first-ever global resolution on kidney health, and researchers completed the world’s first personalized CRISPR therapy given to baby with genetic disease.
Meanwhile, just a few blocks west of the conference, the policy landscape continued to shift. CMS rolled out an aggressive new strategy to accelerate Medicare Advantage audits—adding thousands of coders and expanding reviews to all eligible plans by 2026. The Trump administration and its ‘MAHA’ commission also released a new report on chronic disease in children, raising questions over its framing of trends in cancer, obesity, and aging— and what it left out.1
We’re also testing a shorter recap format this week—fewer words, same Signals. If you make it to the end, I’d love your feedback. Thanks for being here.
In this issue
Global milestone: WHA resolution on kidney health
CMS reboot: New RFI + Medicare Advantage audits
Medicaid overhaul: What the House bill could mean
Breakthroughs in AKI recovery & AI-led discovery
CLTI awareness & new patient-centered resources
Highlights from the Kidney Innovation Conference
Community voices on dignity, advocacy & access
20 new roles across Sanofi, Bayer, Vantive, & more…
Signals
This week’s top stories reveal a moment of reckoning—and opportunity—in kidney and chronic care: from kidney disease finally earning global health recognition, to CMS opening the door for bolder value-based models, to a sweeping House bill that could upend Medicaid for millions. Here’s what’s happening and why it matters.

1. Kidney Disease Makes Global Health History
The World Health Assembly has officially passed the first-ever global resolution on kidney health, recognizing chronic kidney disease as a growing public health issue. Led by Guatemala and co-sponsored by several Member States, the resolution urges countries to integrate kidney care into national health strategies, prioritize early detection and prevention, and strengthen kidney services through primary care systems. This landmark move places kidney disease alongside other major noncommunicable diseases (NCDs) in global health policy for the first time. While the resolution is non-binding, it sets a precedent for funding, program design, and global collaboration. As universal health coverage efforts expand, advocates hope this resolution will drive more visibility, research investment, and equitable access to care for the 850+ million people affected by kidney disease worldwide.2
2. CMS Asks Us How to Unblock Care Innovation
On May 13, CMS unveiled a new strategic direction for the Innovation Center, emphasizing evidence-based prevention, consumer engagement, and tech-enabled care. The 2025 strategy—aligned with the Trump administration’s “Make America Healthy Again” agenda—marks a notable shift from broad participation to performance-focused models with greater downside risk. Accompanying the strategy is a Request for Information, seeking input on how federal law can better support digital health, data sharing, and patient-driven care. Future CMMI models are expected to focus on site-neutral payments, Medicare Advantage redesign, and stronger alignment across payers. Critically, all models will now require downside risk participation. Stakeholders should anticipate more stringent benchmarks, reduced state-level rate setting, and a stronger role for private sector partnerships. While the Innovation Center has not yet set a coverage goal akin to past “100% ACO” mandates, the tone is clear: innovation must be fiscally accountable, consumer-centered, and digitally enabled.3
3. GOP Medicaid Cuts and Budget Bill Updates
In a razor-thin 215–214 vote, the House passed Republicans’ sweeping reconciliation bill—marking the most significant attempt to restructure Medicaid since its founding. The legislation cuts an estimated $700 billion from Medicaid over 10 years, primarily by requiring beneficiaries to meet new work-reporting mandates starting in 2026. The Congressional Budget Office estimates 7.6 million people would lose Medicaid coverage, with another 4 million losing ACA plans—reversing nearly half the coverage gains since 2010. The bill also extends Trump-era tax cuts, which the CBO projects will add $3.8 trillion to the federal deficit over the next decade. Republicans argue the cuts combat fraud and preserve benefits for the neediest, while Democrats and health leaders warn the bill will gut safety-net programs, close hospitals, and worsen health outcomes. For kidney patients—nearly half of whom rely on Medicaid—these proposals represent a potentially massive disruption in coverage and care continuity.4
Visual of the Week

Biobanks and kidney research. This global snapshot of genomic biobanks and studies reflects both the scale and complexity of modern data infrastructure in healthcare—and the conversations at last week’s Kidney Innovation Conference made clear that we still have work to do. In the pediatric trials workshop, researchers, industry, and patients discussed the challenges of consent, data sharing, and alignment between foundations and commercial stakeholders. A major theme: patients want follow-through—”tell us where the data went, how it went, and who it helped.” We’ll be exploring this topic further in an upcoming Signals brief.
News
Medtronic to spin off its diabetes business: The company will separate its insulin pumps and glucose monitors unit into a standalone firm amid broader portfolio streamlining. The diabetes unit employs more than 8,000 people worldwide and represented 8% of Medtronic’s fiscal year 2025 revenue (Press, Becker’s, MedTech Dive).
Lupin launches generic tolvaptan for ADPKD with 180-day exclusivity: The FDA-approved launch offers a lower-cost alternative to Jynarque for slowing kidney decline in adults with autosomal dominant polycystic kidney disease (ADPKD), entering a $1.4B U.S. market with first-to-file status (BW Healthcare World).
Hinge Health pops 17% in public debut, but at half its 2021 valuation: The digital physical therapy firm closed its first trading day at $3B—down from its $6.2B Series E valuation in 2021—joining a wave of down-round IPOs reshaping expectations in digital health (CNBC, TechCrunch).5
Dialysis giants DaVita and Fresenius face antitrust lawsuit: A union health benefits fund is suing the companies for alleged collusion and price inflation in dialysis services to the tune of billions of dollars (Reuters, Bloomberg, Denver BJ).
DaVita hit by ransomware attack: On April 12, DaVita reported a ransomware breach that encrypted parts of its network; while patient care was unaffected, the Interlock gang has since claimed responsibility and allegedly leaked 700,000 files to the dark web. The attack follows similar breaches at Fresenius (500K patients) and UnitedHealth (100M affected) in recent years, highlighting escalating cybersecurity threats across third-party healthcare networks (Healthcare Brew, Reuters).
CMMI releases new strategy to advance MAHA agenda: The CMS Innovation Center's 2025 strategy focuses on prevention, patient empowerment, and competition—signaling a shift toward site-neutral payment, broader provider inclusion, and upcoming model redesigns aligned with these pillars (CMMI, AAMC, Fierce).6
Research
First-in-human base editing therapy shows early success in rare metabolic disorder: NIH-funded scientists just achieved a major milestone in the evolution of personalized therapies for rare & ultra-rare inborn errors of metabolism (NEJM).
USC engineers develop kidney-targeted gene therapy platform: Researchers created a nanoparticle-based delivery system for gene therapies using engineered extracellular vesicles to target kidney and cardiovascular disease (USC Viterbi).
Deep learning predicts lupus nephritis treatment response: A multistain pathology-based AI model showed potential for personalized risk stratification in LN patients (LinkedIn post).
New review highlights complexity of kidney recovery after AKI: A systematic review synthesizes evidence on the biological, clinical, and environmental factors influencing AKI recovery, revealing both progress and persistent uncertainty in how these factors interact—offering guidance for improving outcomes in post-AKI care (Cardiorenal Medicine).
New insights on CLTI awareness and amputation prevention: Leaders in PAD and vascular care emphasize the need for culturally competent, community-driven outreach built on experience, exposure, and education—highlighting models like Get a Pulse on PAD that center patient voices and scalable storytelling approaches (EV Today, h/t Terry Litchfield).
AI agents identify novel dry AMD treatment in 10 weeks: FutureHouse’s “Robin” system—using a closed-loop of AI agents—discovered Ripasudil as a candidate for dry age-related macular degeneration, marking a milestone in automated scientific discovery (FutureHouse).
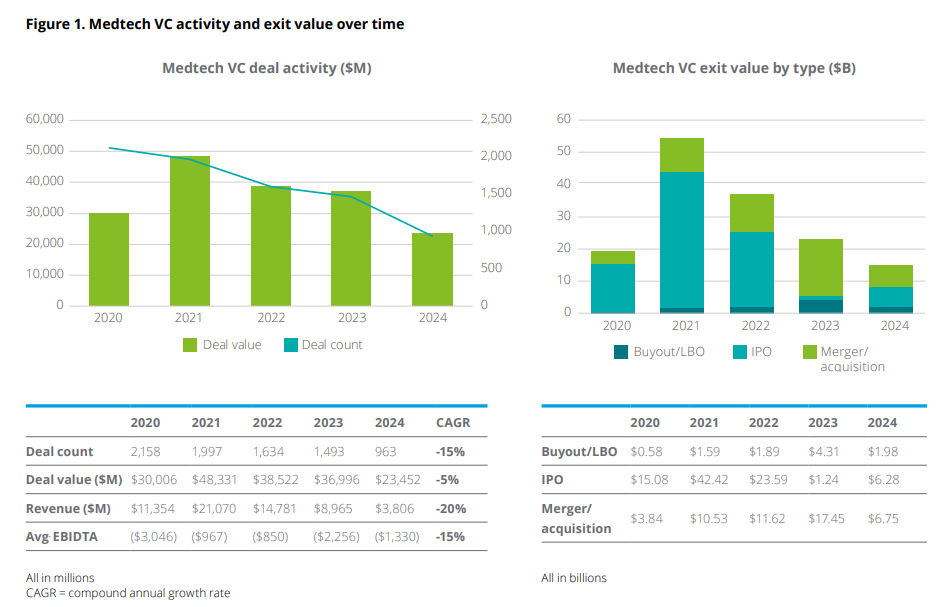
Deloitte explores “build-to-buy” as a rising model in medtech: A new report highlights the growing appeal of milestone-triggered acquisition deals between strategics and startups—offering early-stage medtech companies financial stability and R&D leverage, but often with capped upside and no guaranteed buyout (Deloitte).
Community

Full house at the Kidney Innovation Conference pediatric trial workshop: Researchers and advocates came together to explore how data extrapolation can unlock new therapies for kids with kidney disease (LinkedIn).
Reflections on CMS’s open call for feedback: Value-based care advocates celebrated CMS’s new RFI as a rare chance to shape the regulatory future of coordinated, tech-enabled chronic care (LinkedIn).
A must-read dialogue on dignity and dialysis: A powerful essay by Dr. Jeffrey Gold sparked an in-depth public conversation with Jeff Parke, a dialysis patient of 30 years, about why U.S. kidney care continues to lag behind global peers—and what meaningful reform must look like; Tom Mueller calls it “essential reading” for anyone serious about change in kidney care (LinkedIn).
A family story of shared sacrifice and living donation: STAT published a moving personal piece on two sisters who each donated a kidney to their brother—a powerful testament to love and the life-changing impact of living organ donation (STAT).
Healthy.io hits 300,000 test milestone: The company announced over 300,000 at-home urinalysis tests performed through its digital health platform, a major step in expanding kidney screening access outside the clinic (LinkedIn).
Milestone moment for nephrology authorship: The 6th edition of Handbook of Dialysis includes four new chapters co-authored by rising leaders in kidney care—described as a “full-circle” moment by Dr. Tushar Vachharajani (LinkedIn).
A must-bookmark VBC lecture series: Dr. Paulius Mui spotlighted a free set of educational videos covering the finer points of value-based contracts, risk adjustment, attribution, and bundled payments—essential context for anyone navigating VBC from the outside in (XPC Courses).
What exactly is a “patient advocate”: In a recent post, Dr. Macey Levan asks the community to reflect on the meaning of the term “patient advocate” and many ways people identify with the goals, actions, and experiences of each (LinkedIn).
Events Calendar
European Nephrology Conference (May 26-27 in Rome, Italy)
European Renal Association (June 4-7 in Vienna, Austria)
AMGA Value Roundtable (June 9-10 in Washington, DC)
LSI Asia Summit (June 10-13 in Singapore)
International Podocyte Conference (June 11-13 in Hamburg)
Benesch Nephrology & Dialysis Conf (June 26 in Chicago, IL)
Jobs
Director, Generative AI — Natera
Sales Manager – Digital Health — Vantive
Lead Data Scientist - Healthcare Delivery — Oak Street Health
VP, Member Experience Ops & Innovation — Cityblock Health
Director, Process Development — ProKidney
Manager, Patient Access — Intermountain Health
Health Economic Policy & Reimb Analyst — Medtronic
Director, Global Logistics — Akebia Therapeutics
Principal Reimbursement Analyst - RDN — Medtronic
Transplant Medical Science Liaison — Sanofi
Global Program Clinical Head - Renal — Novartis
Biostatistics Leader - CVRM — Roche
Director of Drivers of Health — Blue Cross NC
Browse 100+ more at jobs.signalsfs.com…
This newsletter brings together 15,000 kidney professionals in 50 countries every month around topics in kidney health and innovation. Please consider sharing it with your colleagues and friends. Thank you.
Thoughts?!
The MAHA Report. (whitehouse.gov/maha)
Full text: Reducing the burden of noncommunicable diseases through promotion of kidney health and strengthening prevention and control of kidney disease.
Analyzing the Expanded Landscape of Value-Based Entities: Implications and Opportunities of Enablers for the CMS Innovation Center and the Broader Value Movement. Research from HMA and LP VBP experts segments and sizes the growing enabler market, considering benefits and risks, and proposing guiding principles and policy recommendations for the CMS Innovation Center. The in-depth HMA report analyzes the landscape of emerging value-based entities and the implications for accelerating the adoption of accountable care.
H.R.1 - One Big Beautiful Bill Act (Congress.gov)
"Some People Are Lazy Dirtbags" is the Magic Phrase that Lets Democrats Talk About Medicaid Work Requirements. “Many on the left think that Medicaid work requirements are bad policy; their main point is that the cost “savings” come overwhelmingly from eligible Medicaid recipients who fail to navigate bureaucratic hurdles. I agree with those analyses — adding a work requirement to Medicaid is like “family style” dining in that it sounds great but sucks in practice.1 A lot of deserving people will get hurt by the effort to root out the undeserving, and the government won’t reduce costs so much as move them around. Explaining why Medicaid work requirements are bad policy takes a minute…” (H/t to Jeff Maurer for writing and MG for sharing this one with me. It certainly helped me wrap my mind around how we talk about the details.
The Hinge Health S-1 Breakdown. If you want the full story on Hinge look no further than Blake Madden’s recent piece. In typical Hospitalogy fashion, Blake breaks down the problem, programs, operations and financing in a way that’s easy to digest for those following the digital health and hospitals spaces. Great work, Blake!
CMS Innovation Center Strategy to Make America Healthy Again. It’s worth reading Center Director Abe Sutton’s piece that CMMI published on May 15, 2025. There’s also a nifty little ‘Where Health Care Innovation is Happening’ tool so you can see current payment and service delivery models at the state level.
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)