Signals Recap: Prioritizing Kidney Health on the World Stage and Here at Home
Your biweekly collection of news, research, funding & community voices shaping the future of global kidney health
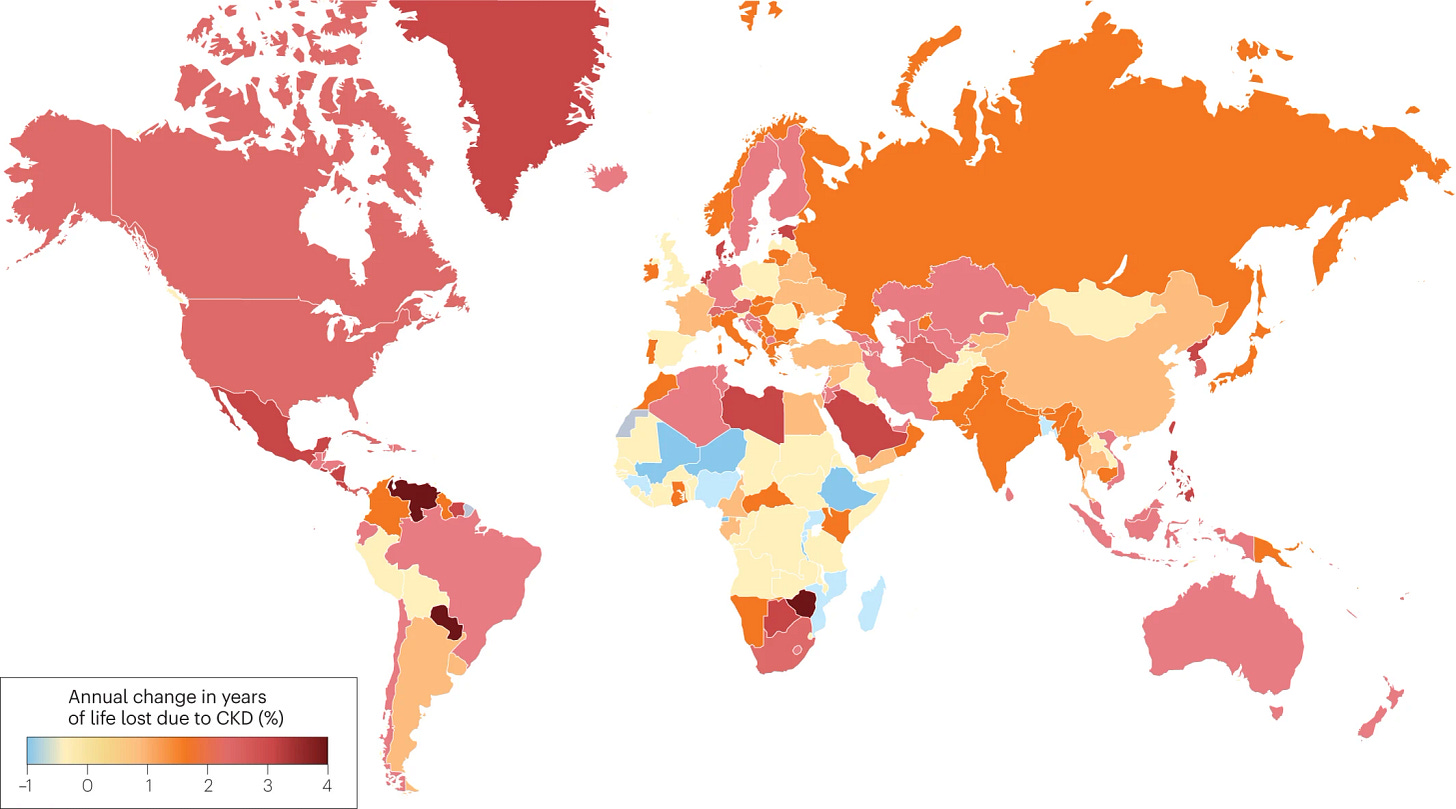
As we head deeper into 2025, the landscape around kidney health, innovation, and policy is shifting quickly—and not just here in the United States. On May 19, the World Health Assembly will gather for its 78th meeting to decide how to allocate its (shrinking) resources toward the world’s most urgent health needs. A recent editorial in Nature argues that we have a golden opportunity to recognize and rein in the largely overlooked burden of chronic kidney disease—now one of the fastest-growing causes of premature death globally, projected to become the fifth leading cause of years of life lost by 2040.1
Here at home, we’re also navigating a thick fog of uncertainty that continues to spread far and wide. A huge thank you to Miriam Godwin from the National Kidney Foundation for lending her expertise to help us unpack the potential impact of the leaked FY2026 HHS budget proposal. It’s a powerful reminder of how much advocacy, research, and innovation remain essential as the ground moves beneath us.
Before we dive in: a fun surprise—Signals was named a Bestselling newsletter on Substack and landed at #60 on Substack’s Rising 100 Health & Wellness list. Thank you for helping put global kidney health "on the map." It’s encouraging to see topics like kidney disease, research, policy, innovation, and investment earn a seat at the table alongside broader conversations about health.
Thank you for being here with us. If you find this recap valuable, consider forwarding it to a colleague or friend who’s working to make kidney health better for all.
In this issue
What a proposed $40B cut to HHS could mean for kidney care
FDA Commissioner appoints new leadership team
First clinical trial using pig livers for liver failure approved
MIT study highlights tradeoffs in kidney transplant allocation
Kidney disease advocacy ramps up ahead of WHO vote
Strive Health expands partnership with Aetna
Paragonix hits 100th kidney transplant milestone
New research on PD training, acute dialysis costs, and liver allocation
Breakthroughs in kidney gene therapy and robotic transplant milestones
TEDx, NEJM Catalyst, and podcast highlights from across the community
New roles at Diality, CareDx, Novartis, NKF, Eurofins, and more
See 50+ open kidney roles at jobs.signalsfs.com
This edition of Signals is brought to you by Natera. With over 130,000 patients tested with the Renasight™ test, Natera has the largest commercially available kidney disease database that can help accelerate research and drug development in the space. Discover how Natera’s Renasight™ database helped accelerate an Alport Syndrome clinical trial by 3x. Thanks team!
Signals
What a Proposed $40B Cut to HHS Could Mean for Kidney Care
Summary: Last week, a leaked FY2026 budget proposal outlined plans to cut $40 billion—about one-third—of the Department of Health and Human Services’ discretionary funding. Major programs would be consolidated, eliminated, or reorganized, including the dissolution of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) into a broader National Institute on Body Systems, the elimination of the KidneyX innovation accelerator, and a shift away from chronic disease prevention at the CDC. These changes could have far-reaching implications for kidney health research, innovation pipelines, and access to federal funding streams that have supported progress over the last decade.
Thoughts: While budget proposals often face an uphill battle in Congress, the sheer scale and focus of this one sends an important signal about shifting federal priorities. Consolidations like those proposed for NIDDK could dilute disease-specific funding, while the elimination of KidneyX would dismantle a proven model for accelerating kidney innovation. Chronic disease efforts—already underfunded compared to infectious disease—would likely take another step backward. It's a moment that calls for close attention and collective advocacy from the kidney community.
A big thanks to Miriam Godwin, Vice President of Health Policy at the National Kidney Foundation, for sharing her perspective and helping us break this down. You can listen to Miriam’s quick take above and get more details in our full brief below.
What do you think? What are you watching most closely as this budget proposal unfolds? How should the kidney community prepare for these potential changes?
Visual of the Week
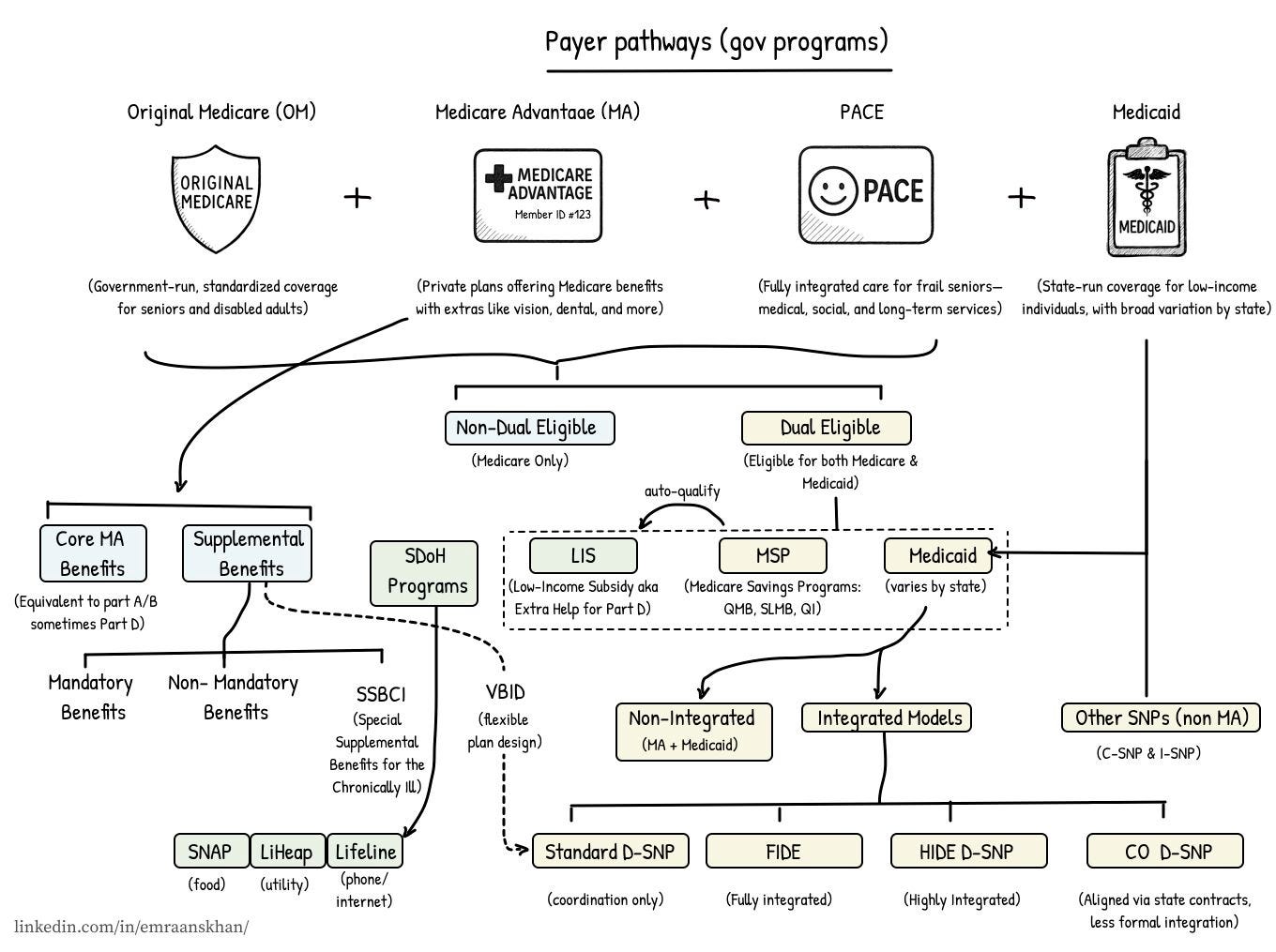
Behold: A “Simplified” U.S. Payer Landscape. This week’s visual comes from Emraan Khan, who captured the sprawling complexity of U.S. public payer pathways across Medicare, Medicaid, and PACE programs. Every box on the chart represents a real-world system someone has to navigate—often while sick, aging, or facing financial hardship. It’s a humbling reminder of how fragmented access to care remains, and how much work lies ahead to build systems that are truly navigable and equitable. The thoughtful comments on Emraan’s post highlight just how invisible and burdensome these barriers can be for patients—and how important collaboration and shared understanding will be to fix them.
For kidney patients, who may qualify for multiple programs but must navigate dialysis, transplant, or complex specialty care at the same time (if they’ve been referred), making these pathways simpler isn't just policy work—it’s a critical lifeline.2
News
Dr. Robert Montgomery was named to the TIME 100 Most Influential list for revolutionizing organ transplantation through innovations like laparoscopic kidney donation, domino paired donations, and advancing xenotransplantation. His work has expanded access to life-saving organs and shaped the future of transplant medicine (TIME).
Paragonix Technologies announced a milestone 100th kidney transplant case using its FDA-cleared KidneyVault™ Portable Renal Perfusion System, reflecting the continued adoption of mobile, data-driven organ preservation. As of today, 12 OPOs stock the device, including Tennessee Donor Services, which serves 6 million people across Tennessee and Virginia (Business Wire).
The FDA approved a first-of-its-kind clinical trial testing whether gene-edited pig livers can externally filter blood in patients with sudden liver failure. An estimated 35,000 Americans are hospitalized for acute liver failure each year, facing death rates as high as 50%, with few treatment options available (NBC News).
Strive Health expanded its partnership with Aetna, adding Medicare Advantage members in Connecticut and Ohio (builds on existing coverage in Illinois, Indiana, and Michigan). The company also named Paul Marchetti as President and promoted Jen Browne to Chief Operating Officer as it scales operations to support growth (LinkedIn, Strive Health, h/t Will Stokes).
Sonavex shared progress on its MAFASA clinical trial, partnering with Dr. Christopher Mitromaras and the team at Atrium Health and the Sanger Heart & Vascular Institute to study the the EchoMark®/EchoSure® System for AVF diagnostic ultrasound (LinkedIn, h/t John Rappe).
University of Toledo scientists found that activating the melanocortin 5 receptor (MC5R) could reduce kidney damage, offering a more targeted approach to treating glomerular diseases and reducing proteinuria without relying on broad immunosuppressants. Their NIH-funded research was just published in Kidney International’s May issue (University of Toledo).
Shraddha Kalgutkar’s transplant survival highlights organ preservation. Mayo Clinic used innovative warm perfusion technology ("liver in a box") and mobile ECMO support to perform a complex transplant that saved Shraddha Kalgutkar’s life, showcasing the power of combining advanced preservation methods with patient-centered critical care (Mayo Clinic).
Policy
FDA Commissioner Marty Makary announced three new agency leaders this week, including Lowell Zeta as deputy commissioner for strategic initiatives and Craig Taylor as the acting chief information officer. Zeta served as a senior adviser to the commissioner during the first Trump administration, and helped lead the FDA’s 2020 initiative to evaluate its Covid-19 response (STAT News).
FDA officials warned that staff reductions tied to the new Department of Government Efficiency (DOGE) restructuring have led to missing or delayed updates in drug safety and manufacturing databases. Experts say these databases are critical for clinicians, researchers, and supply chains, raising alarms about patient safety and transparency risks (Axios).
STAT News launched a day-by-day interactive timeline documenting major policy changes impacting science, health agencies, and global health, including funding cuts, agency reorganizations, communication freezes, and executive orders reshaping public health infrastructure (STAT News).
AdvaMed published an “AI Policy Roadmap” urging Congress and federal agencies to modernize regulations, payment models, and privacy protections to accelerate access to AI-enabled medical devices. Over 1,000 AI-authorized technologies have been cleared by the FDA to date, with future policies seen as critical to expanding patient access and innovation (AdvaMed, h/t Jed Dadson).
How should we prioritize patients waiting for kidney transplants? MIT researchers found that current kidney transplant practices generate 9.29 additional life-years for recipients on average, but that figure could rise to 14.08 with optimized allocation favoring healthier patients — highlighting a policy tradeoff between prioritizing the sickest patients and maximizing overall survival gains (MIT Press).
Research
A new chart collection from the Peterson Center on Healthcare-KFF Health System Tracker highlights that chronic kidney disease (CKD) prevalence in the U.S. has remained substantially higher than in peer nations over the past three decades, with a 24% higher prevalence rate than comparable countries as of 2021 (Peterson-KFF Health System Tracker).
A new Nature editorial argues kidney disease must be recognized as a global health priority. Its authors call on the World Health Assembly to formally recognize chronic kidney disease as a major non-communicable disease (NCD), citing its global prevalence (674 million people), rapid growth, and links to premature mortality (Nature, h/t Helen Yeh).
How do PD training methods and educational interventions impact on PD outcomes in adult patients? A narrative review highlights gaps in the evidence base for peritoneal dialysis (PD) training interventions but suggests that individualized training approaches, pre-training assessments, and consistent outcome measures may improve PD outcomes in adult patients (Journal of the International Society for Peritoneal Dialysis).
An updated review of Membranous Nephropathy (MN) discusses recent advances in antigen mapping, genetic and environmental risk factors, and evolving therapeutic strategies, emphasizing its status as a leading cause of nephrotic syndrome in adults and the growing clinical role of PLA2R antibody testing (Indian Journal of Nephrology, h/t Edgar Lerma).
A new case report published in AJT highlights the growing role of genetic testing in kidney transplant clinics and the need for collaboration among nephrologists, cardiologists, and genetic counselors when evaluating candidates with hereditary transthyretin (TTR) amyloidosis (AJT, h/t Yasar Caliskan).
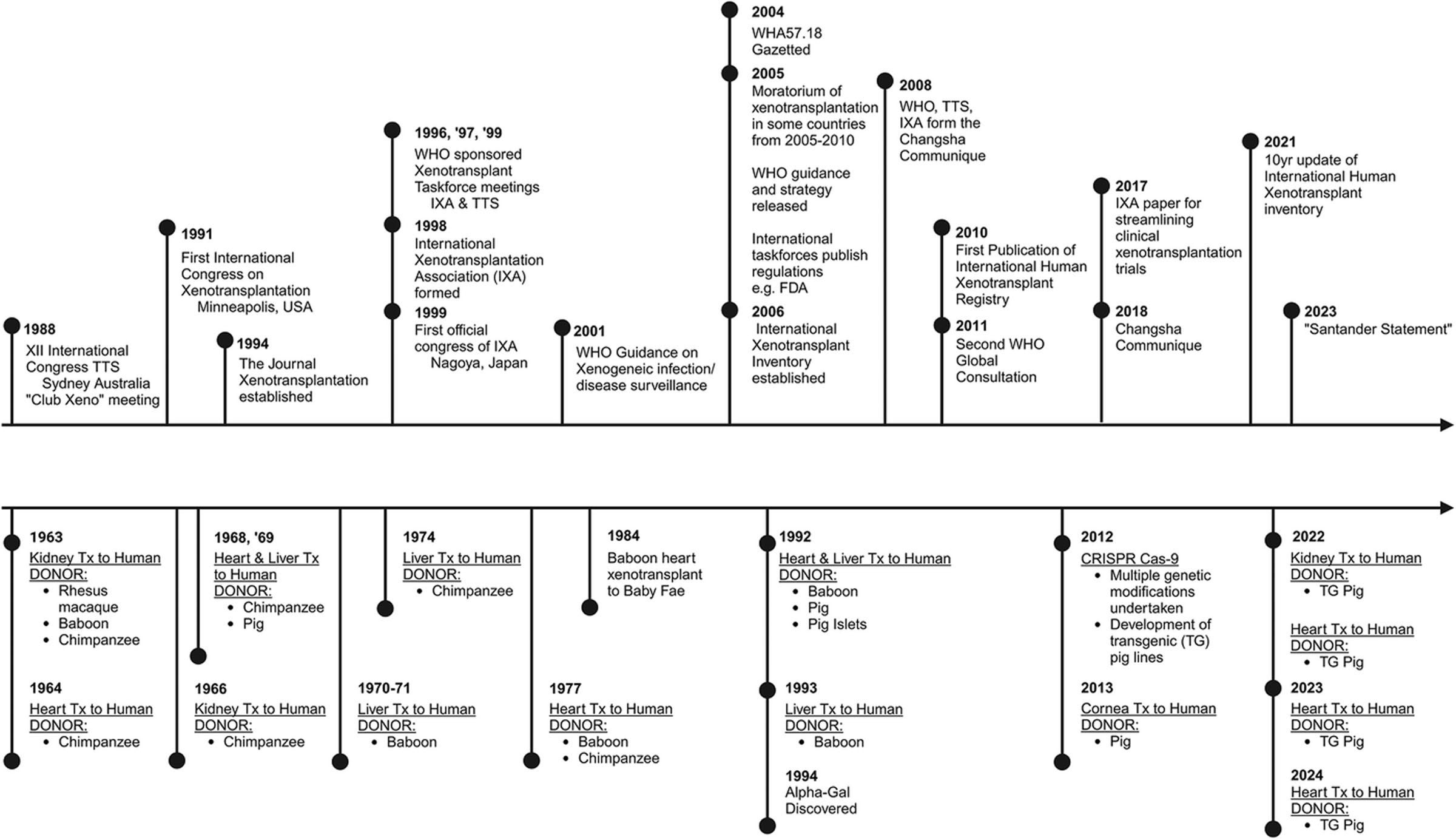
A new position paper from the International Xenotransplantation Association reviews the history, regulatory milestones, and technical innovations that have enabled recent clinical translation of heart and kidney xenografts, emphasizing emerging frameworks for ethical and safe application-specific standards (Transplantation, see milestones below).
If you are offered a choice to participate in a clinical trial - do you or your family know what questions to ask? A new survey led by the Kidney Health Initiative and National Kidney Foundation seeks patient and care partner input to help inform clinical trial decision-making for kidney xenotransplants, building on prior patient-focused research and a collaborative meeting with the FDA (KHI, h/t Mark Lim).
A new study from Norman Regional Health System found that transitioning to an in-house dialysis care model at a regional acute care hospital in Oklahoma increased treatment volume by 400% and improved successful dialysis completion rates from 73.7% to 97.5% over nine months (Healio).
A new study found that discontinuation of IV etelcalcetide following a US reimbursement policy change led to a rapid and sustained increase in parathyroid hormone (PTH) levels among hemodialysis patients, with particularly pronounced effects among Black patients, raising concerns about unintended clinical disparities (CJASN, h/t Neph Times).
A new simulation study found that shifting to survival benefit-based liver transplant allocation would increase post-transplant survival by only 18 days on average, while potentially leading to 400 additional waitlist deaths annually, supporting the continued use of sickest-first allocation (Hepatology).
A new perspective piece outlines how digital health technologies (DHTs) can expand decentralized clinical trials by enabling continuous remote data collection, improving participant access and engagement, and supporting the development of novel clinical trial endpoints (JAMA Health Forum).
Community

Vincent Ko recently highlighted Nephrogen, a new biotech developing next-generation gene therapies for kidney diseases, including a single-administration treatment for autosomal dominant polycystic kidney disease (ADPKD) using a novel capsid delivery platform 100x more efficient than standard AAVs (LinkedIn, h/t Vincent Ko).
Dr. Tarek Alhamad, Medical Director of Transplant Nephrology at Washington University in St. Louis, celebrated a milestone of 45 kidney transplants performed in a single month, marking a new record pace for the program (LinkedIn, h/t Tarek Alhamad).
Anna Kaltenboeck shared highlights from ATI Advisory’s 2024 Biopharma Year in Review, noting continued R&D momentum, a shift toward earlier-stage deals, the rise of China-based biotech licensing, and growing focus on the Medicare Part D redesign and its projected impact on biopharma revenues (LinkedIn, h/t Anna Kaltenboeck).
Dr. Bijal Patel celebrated a major milestone for Balboa Nephrology and Sharp Memorial Hospital, where Dr. Marquis Hart performed San Diego’s first robotic-assisted kidney transplant — an exciting step forward in surgical innovation and patient care for the community (LinkedIn, h/t Bijal Patel).
NephCure recognized Dr. Martin Pollak and his team for their decades of groundbreaking work advancing research and hope for the rare kidney disease community (LinkedIn, h/t NephCure).
Renee Aguiar-Lucander, former CEO of Calliditas Therapeutics, announced she has taken on the role of CEO at Hansa Biopharma to lead the development of its proprietary IgG-cleaving platform (LinkedIn, h/t Renee Aguiar-Lucander).
Kate de Lisle highlighted new analysis from Rob Mechanic and the Institute for Accountable Care on TEAM, CMMI’s forthcoming mandatory episode-based payment model set to launch in 2026, which will require closer collaboration between hospitals, specialists, primary care, and ACOs (LinkedIn, h/t Kate de Lisle).
The team at 34 Lives marked the one-year anniversary of their first rescued kidney transplant, reporting that their original study goal of 80 rescued kidneys has been surpassed with 125 completed transplants to date, in partnership with OPOs and transplant centers nationwide (LinkedIn, h/t 34 Lives).
Nick Bartz, Co-Founder and CEO of Kairon Health, shared reflections on the persistent challenges in value-based care (VBC) contracting, highlighting how one-size-fits-all approaches often fail to account for real practice economics and operational realities. His post is a great reminder of the need for more tailored transition strategies as practices navigate the shift from fee-for-service to VBC models (LinkedIn, h/t Nick Bartz).
Dr. Vimal Mishra, Chief Medical Officer at Dignity Health, shared results from a new NEJM Catalyst paper highlighting UC Davis Health’s Urgent Care at Home model, which served 815 high-risk patients over six months, achieved a >100% ROI, and reduced emergency department visits by delivering digitally enabled, clinically integrated care at home (LinkedIn, h/t Vimal Mishra).

Watch & Listen
Dr. Joe Scalea, Vice Chair and Professor of Surgery at MUSC, delivered a powerful talk at TEDxCharleston last week titled ‘Four Reasons to Live.’ He reflects on lessons from transplant patients about what makes life meaningful, drawing on experiences from his work caring for patients facing organ failure and new chances at life (LinkedIn, h/t Joe Scalea).
Dr. Erick Bricker joined Stacey Richter on the Relentless Health Value podcast to explain how hospital systems leveraged provider stop-loss reimbursement clauses and chargemaster manipulation to drive up costs for employer-sponsored plans—highlighting why recent insurer strategies to control these dynamics have started to fail (LinkedIn, h/t Erick Bricker).
Events Calendar
ANNA National Symposium (May 1-4)
KHI Kidney Innovation Conference (May 21-22)
World Transplant Congress (August 2-6)
ASN Kidney Week (November 5-9)
VEITH Symposium (November 18-22)
Jobs
Senior Director, US Patient Advocacy at Lundbeck
Transplant Laboratory Tech II at University of Utah
Director, State Government Affairs at hims&hers
Product Marketing Manager at Diality
Solid Organ Transplant Clin Dir of Ops at Tufts MC
Customer Implementation Manager at Healthie
Senior Director, SEC Reporting & Accounting at CareDx, Inc.
Organ Health Specialist at Natera
Commercial Dev Manager, Digital Tech at Medtronic
Associate Director, Health IT Strategy at Novartis
Market GM, Patient Care Solutions at GE Healthcare
Director, Special Projects (ROPS) at DaVita
Browse more at jobs.signalsfs.com…
Moving You Forward
Thank you for reading Signals Media, the leading newsletter for kidney innovation, ideas, and investment. We recently launched Signals Advisory to help companies, investors, and organizations navigate the growing, complex kidney health landscape. Learn more and share your next milestones here.
Francis, A., Harhay, M.N., Ong, A.C.M. et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat Rev Nephrol 20, 473–485 (2024). https://doi.org/10.1038/s41581-024-00820-6
A systematic review of 17 studies found that patient navigators for CKD and kidney failure improved transplant workup, peritoneal dialysis utilization, and patient knowledge, though overall outcomes varied. Navigators came from diverse backgrounds and focused mainly on education and support, but few studies assessed cost-effectiveness or patient experience, and risk of bias was common. High-quality randomized trials are needed to better evaluate navigator program impact and sustainability (Kidney Medicine).
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)