When government regulation goes too far — or misses the mark — the effects can take a human toll. In dialysis care, where more than 70% of patients rely on Medicare, those effects are magnified. Dr. Eugene Lin, a nephrologist and policy researcher, joins us to explain how well-intentioned regulation has entrenched monopolies, sidelined new entrants, and failed to deliver better outcomes.
In their Health Affairs Forefront article, Drs. Eugene Lin, Ge Bai, and Erin Trish argue that excessive and poorly designed government regulation has entrenched consolidation, stifled innovation, and inflated costs in the U.S. dialysis industry. Using end-stage renal disease (ESRD) as a case study, they show how regulations intended to protect patients and improve quality have instead empowered large dialysis providers, driven up taxpayer spending, and left patients with poorer outcomes. Lin, Bai, and Trish call for simplification of quality programs, removal of market-entry barriers, and curbing anticompetitive practices.1
I invited Dr. Lin to join me here on Signals KOLs to unpack their findings and share pragmatic ideas for building a more dynamic, effective, and equitable dialysis market.
At a time when Medicare Advantage enrollment among beneficiaries with ESRD continues past 50% and value-based models are reshaping upstream care, this is a warning health policy leaders quite literally cannot afford to ignore.
Biography
Eugene Lin is a nephrologist and health economics researcher who focuses on the impact of public policy and federal regulation on kidney care, the provision of dialysis in public and private insurance markets, and transitions of care for patients with kidney disease. He currently serves as an Assistant Professor of Medicine at the University of Southern California (USC). Eugene's research has been featured in high-impact publications such as JAMA, JAMA Internal Medicine, and Health Affairs. His expertise lies in analyzing how value-based care models impact the delivery of kidney care and patient outcomes, making him a key voice in the conversation about healthcare reform.
Keywords
dialysis policy, regulatory capture, Medicare Advantage, kidney care innovation, healthcare consolidation, value-based care
Takeaways
Regulatory capture is real: Large dialysis organizations have become adept at navigating, and benefiting from, complex regulations that smaller players struggle to manage. As Eugene explains, when policy complexity rewards administrative scale over clinical quality, it entrenches incumbents and discourages innovation.23
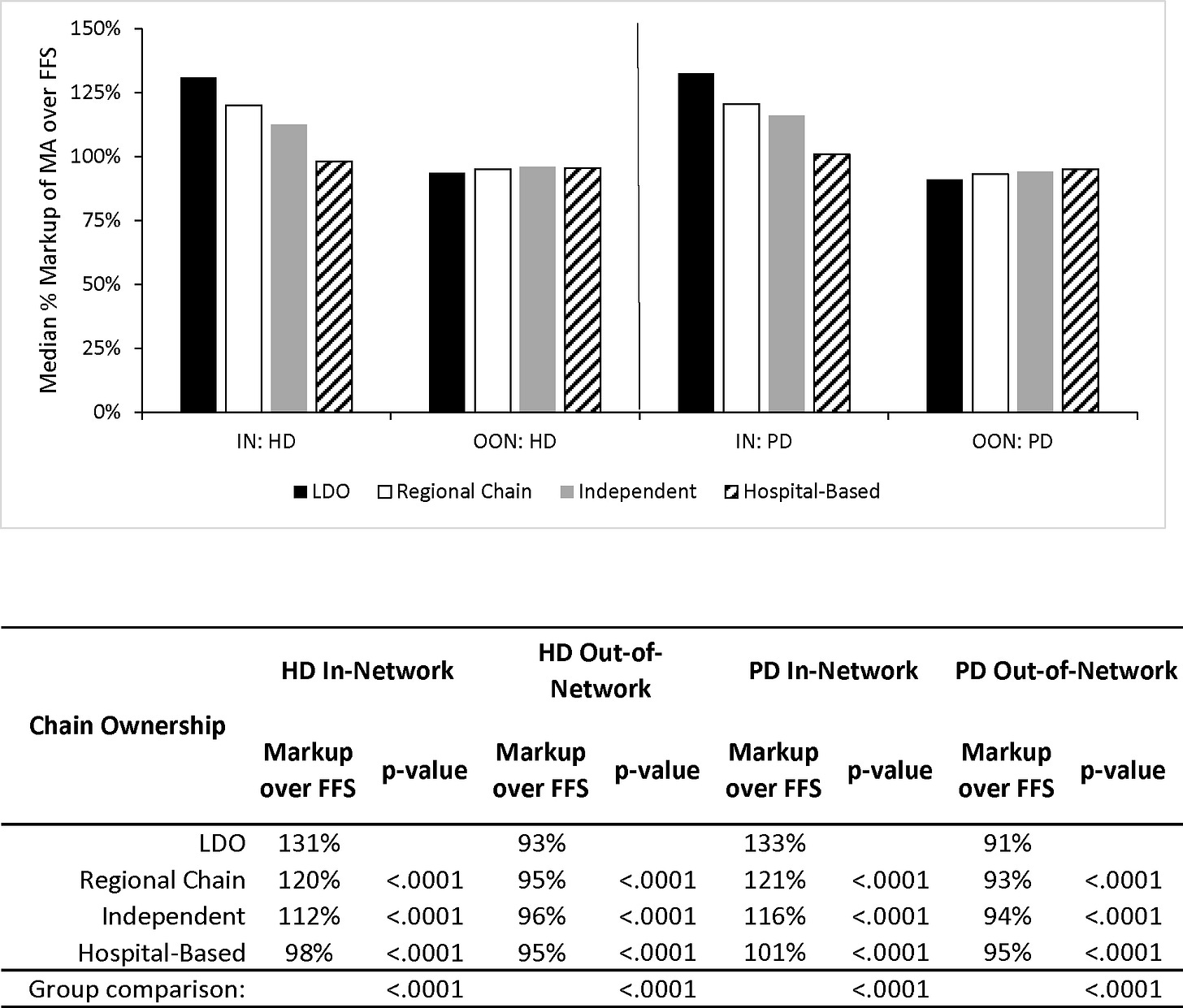
Medicare Advantage is fueling price disparities: Dr. Lin’s research shows that MA plans pay 20–30% more for dialysis than traditional Medicare, largely due to all-or-nothing contracting tactics by large providers. This pricing power drives up taxpayer costs and marginalizes smaller providers who can’t negotiate similar rates.456
Quality measurement has become counterproductive: With overlapping and inconsistent programs like QIP and DFCC, dialysis facilities are drowning in bureaucracy. Rather than improving care, these programs often penalize low-resource clinics and divert attention from what matters most — patient outcomes and clinical excellence.78
Entry barriers are too high: New dialysis providers face a gauntlet of federal certification delays and state-level certificate-of-need (CON) laws, making it difficult to launch innovative care models. As Eugene notes, even well-intentioned entrepreneurs and investors are deterred by the friction and costs of compliance.9
A path forward exists: Instead of adding more rules, Dr. Lin says policy makers should first ask what outdated or redundant regulations can be removed. He suggests banning third-party charity passthroughs, curbing all-or-nothing network deals, and simplifying certification pathways could open the door for meaningful competition and modernization.1011
Chapters
00:21 — Why regulation is a double-edged sword in dialysis
03:45 — Understanding regulatory capture and “ossification”
07:30 — Why small providers struggle under Medicare Advantage
13:55 — Certificate-of-need laws and outdated Conditions for Coverage
15:56 — Why deleting regulations matters more than adding new ones
18:45 — All-or-nothing contracting dynamics and its consequences
24:17 — KCC model takeaways and the role of physician professionalism
28:27 — Payer mix and third-party premium payments
31:22 — What policymakers should delete before regulating more
Discussion Topics
Reactions: This is a complex topic. What are you taking away from this conversation? What resonates, and where should we dig deeper?
Reforms: Which policy changes Dr. Lin mentioned do you believe would help create a more dynamic and competitive dialysis market? Any others?
Care Models: What have you learned from nephrologist-led models that improve access to home dialysis and transplantation?
Leadership: What role should nephrologists play in leading innovation and value-based care programs?
Lin E, Bai G, Trish E. How Regulatory Failures Have Crippled Dialysis Care. Health Affairs Forefront. April 2025. https://www.healthaffairs.org/content/forefront/regulatory-failures-have-crippled-dialysis-care
Lin E, Erickson KF. Payer Mix Among Patients Receiving Dialysis. JAMA. 2020 Sep 1;324(9):900-901. doi: 10.1001/jama.2020.10771. PMID: 32870292.
Himmelfarb J, Vanholder R, Mehrotra R, Tonelli M. The current and future landscape of dialysis. Nat Rev Nephrol. 2020 Oct;16(10):573-585. doi: 10.1038/s41581-020-0315-4. Epub 2020 Jul 30. PMID: 32733095; PMCID: PMC7391926.
Lin E, Ginsburg PB, Chertow GM, Berns JS. The "Advancing American Kidney Health" Executive Order: Challenges and Opportunities for the Large Dialysis Organizations. Am J Kidney Dis. 2020 Nov;76(5):731-734. doi: 10.1053/j.ajkd.2020.07.007. Epub 2020 Aug 5. PMID: 32763259; PMCID: PMC8021090.
Lin E, Ly B, Duffy E, Trish E. Medicare Advantage Plans Pay Large Markups To Consolidated Dialysis Organizations. Health Aff (Millwood). 2022 Aug;41(8):1107-1116. doi: 10.1377/hlthaff.2021.02009. PMID: 35914212; PMCID: PMC11164180.
March 2021 MedPAC Report To Congress (medpac.gov).
Independent dialysis providers face challenges with patient care under Medicare Advantage. September 16, 2024 (Healio).
League RJ, Eliason P, McDevitt RC, Roberts JW, Wong H. Variability in Prices Paid for Hemodialysis by Employer-Sponsored Insurance in the US From 2012 to 2019. JAMA Netw Open. 2022 Feb 1;5(2):e220562. doi: 10.1001/jamanetworkopen.2022.0562. PMID: 35226088; PMCID: PMC8886517.
Trish E, Fiedler M, Ning N, Gascue L, Adler L, Lin E. Payment for Dialysis Services in the Individual Market. JAMA Intern Med. 2021 May 1;181(5):698-699. doi: 10.1001/jamainternmed.2020.7372. PMID: 33749739; PMCID: PMC7985814.
CMS ESRD Measures Manual for the 2025 Performance Period (cms.gov).
“In 2025, facilities are held accountable for a total of 25 total measures, with only 11 overlapping in both programs. Among the 11 measures, only seven have identical specifications, while the remaining four differ in risk adjustment and estimation between the QIP and DFCC. Nine of the 25 measures are risk adjusted, but each uses a different risk-adjustment methodology. Additionally, the patient populations considered for each measure vary—some include the facility’s entire dialysis population, while others are restricted to the entirety of Medicare or traditional Medicare patients.
As more measures are added, the complexity grows. The quality measures manual for both programs ballooned from 150 pages in 2016 to 280 pages in 2025.”
Sheetz KH, Gerhardinger L, Ryan AM, Waits SA. Changes in Dialysis Center Quality Associated With the End-Stage Renal Disease Quality Incentive Program : An Observational Study With a Regression Discontinuity Design. Ann Intern Med. 2021 Aug;174(8):1058-1064. doi: 10.7326/M20-6662. Epub 2021 Jun 1. PMID: 34058101.
Medicare Managed Care Manual: Chapter 4 - Benefits and Beneficiary Protections (cms.gov).
Medicare Program; Contract Year 2021 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, and Medicare Cost Plan Program. Federal Register, Vol. 85, No. 106. Tuesday, June 2, 2020 (govinfo.gov)
Bailey, James B., Can Health Spending Be Reined in Through Supply Constraints? An Evaluation of Certificate-of-Need Laws (08/01/2016). MERCATUS WORKING PAPER, Available at SSRN: http://dx.doi.org/10.2139/ssrn.3211647
Medicare Program; Conditions for Coverage for End-Stage Renal Disease Facilities-Third Party Payment (federalregister.gov).
Health Insurance Premium Program (HIPP) (kidneyfund.org).
Congress should end dialysis companies’ third-party games with insurance coverage. April 29, 2021(STAT)
Conditions for Coverage for ESRD Facilities (govinfo.gov).
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)