Ninety-seven percent of people who reach kidney failure begin dialysis, and nearly 60% won’t live five years beyond it. That journey is defined by late detection, limited options, and high costs to patients and the system alike. For decades, that’s been the norm. Without increased investment in prevention, the total number of patients with kidney failure (ESKD) will likely exceed 1 million by 2030, with nearly forty times as many in earlier stages of the disease.
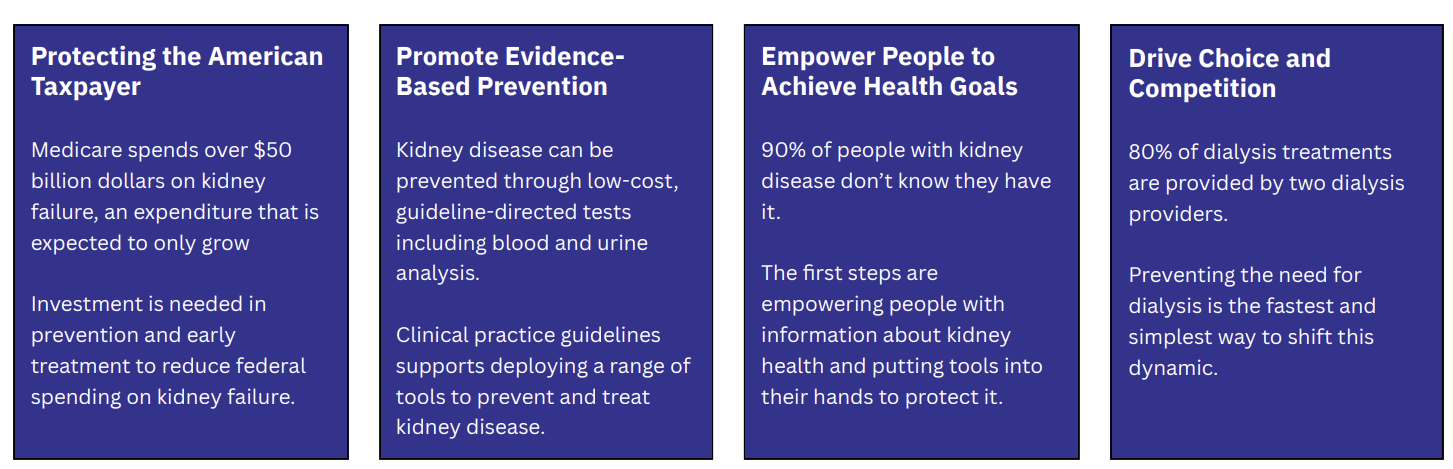
A new report from the Coalition for Kidney Health (C4KH), led by the National Kidney Foundation (NKF), outlines a way to change that story. It offers a practical and tangible roadmap for the Center for Medicare and Medicaid Innovation (CMMI) to expand its focus on prevention, early detection, and patient activation.
In this conversation, Miriam Godwin, Vice President of Health Policy at NKF, and Kevin Fowler, patient advocate and founder of The Voice of the Patient, share how these recommendations build on the 2019 Advancing American Kidney Health Executive Order and align with CMS’s Make America Healthy Again (MAHA) strategy. Together, they describe how value-based care, multipayer alignment, and integrated cardiovascular-kidney-metabolic models can transform the patient journey by shifting from crisis response to prevention, and from managing kidney failure to preserving kidney health.
What’s Inside
Connecting the dots between the 2019 Advancing American Kidney Health Executive Order and CMS’s 2025 Make America Healthy Again strategy.
Q&A
Kevin and Miriam, tell us about your work and how the Coalition for Kidney Health came together.
KF: I’m Kevin Fowler. I run a company called The Voice of the Patient and serve with several volunteer organizations, including the National Kidney Foundation’s Coalition for Kidney Health. I’ve also lived with a kidney transplant for the last 21 years, which gives me a deeply personal view of what kidney patients face.
MG: I’m Miriam Godwin, Vice President of Health Policy at the National Kidney Foundation—and a former CMS-er. I had the good fortune to work on the Kidney Care Choices (KCC) and ESRD Treatment Choices (ETC) models while working at the CMS Innovation Center (CMMI).1
NKF began thinking about convening the Coalition for Kidney Health around 2018. At the time, most national efforts were focused on dialysis, and we wanted to go further upstream: focusing on prevention, early detection, and delaying disease progression. We brought together a multi-stakeholder group of patients like Kevin, innovators, physicians, dietitians, and advocacy partners. Everyone shared the same goal: to talk more about preserving kidney health rather than just managing kidney failure.
Timing was important. We wanted tactical solutions that could be implemented now—recommendations executive agencies could act on immediately to elevate chronic kidney disease. We focused on value-based care because that’s where system transformation happens.
KF: From my perspective, this is a natural extension of the Advancing American Kidney Health (AAKH) Executive Order from 2019.2 That order set the direction, and this paper is about implementation. We’re taking that vision and putting it into practice.
MG: Exactly. It’s helping make good on the promises of AAKH and carrying that momentum forward.
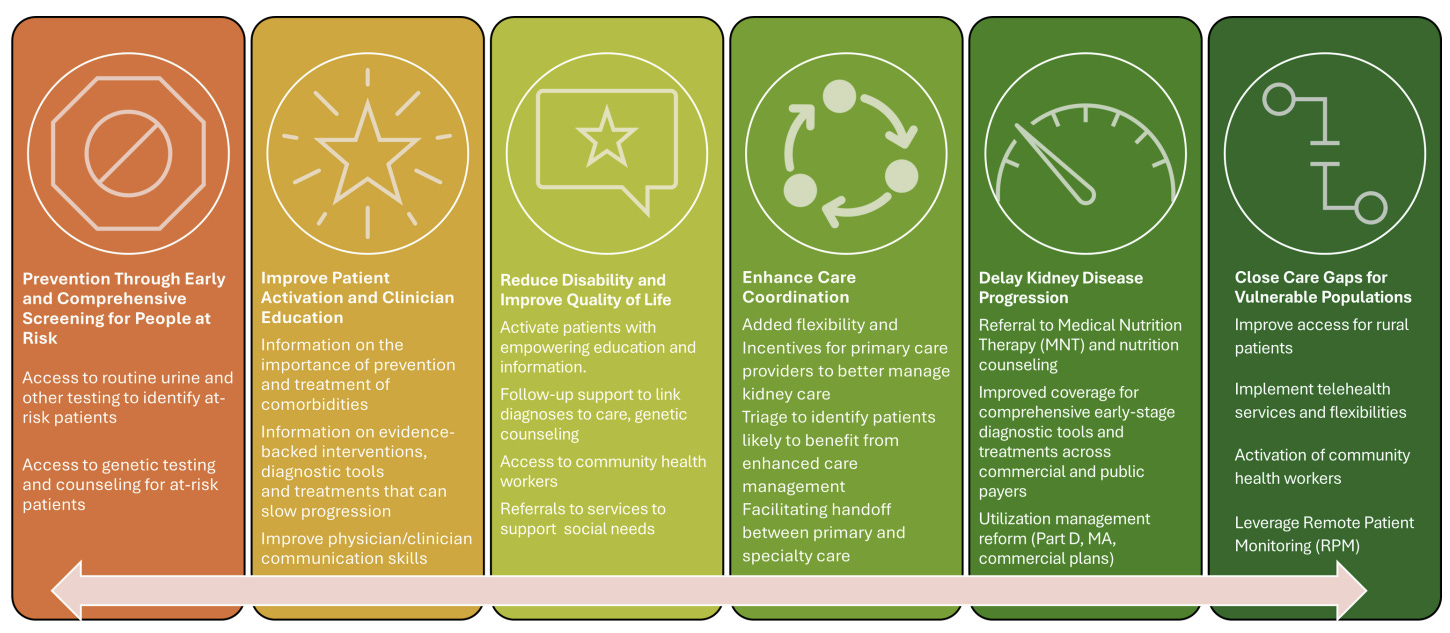
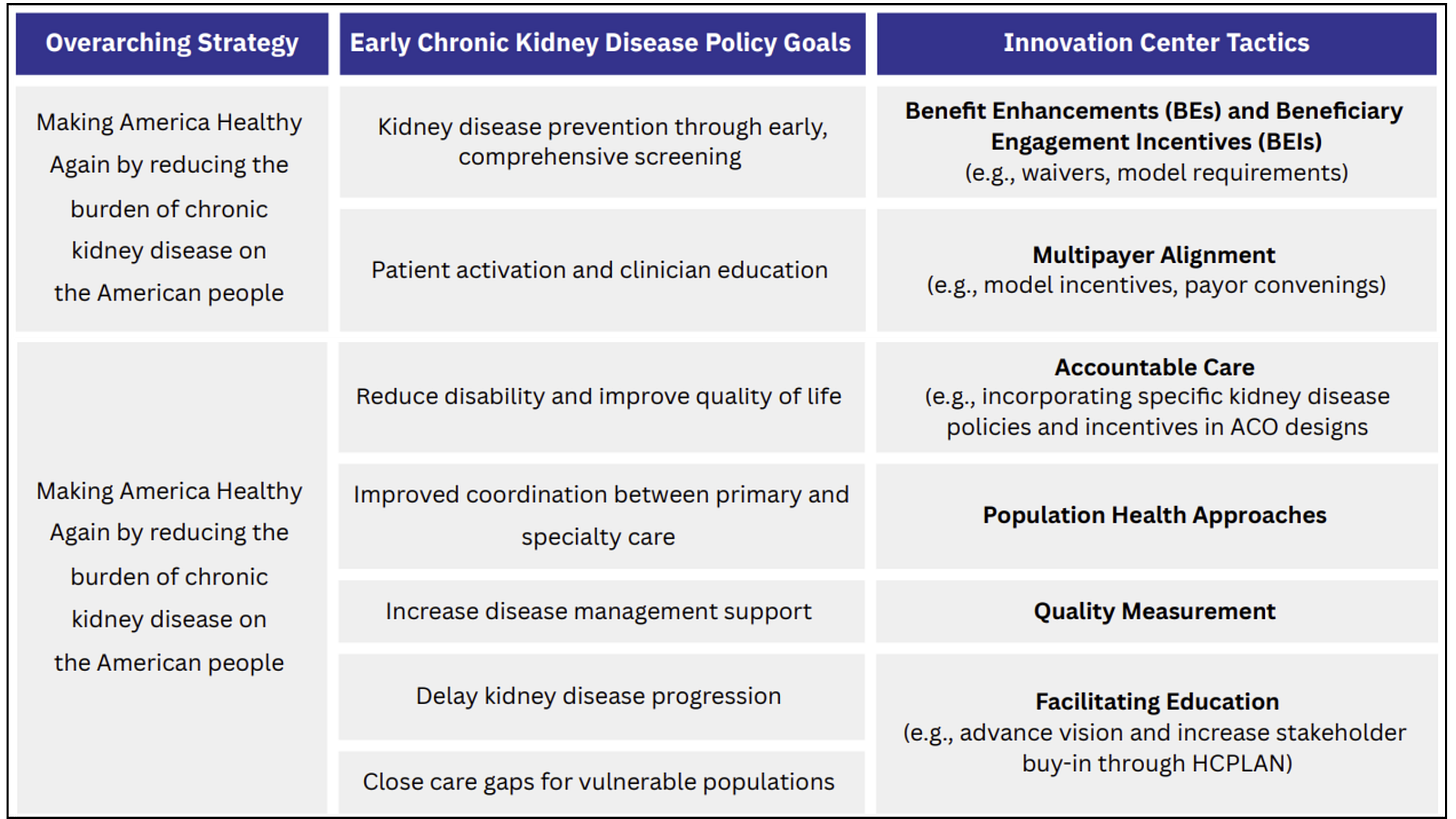
Figure: Early CKD Policy Goals
Why is it so important to move kidney policy upstream?
KF: Anyone living with kidney disease would rather know their kidney health status earlier rather than later. It gives you control. If you’ve ever seen someone on dialysis, it leaves an indelible impression. The five-year mortality rate for people on hemodialysis is 60%, which is unacceptable. The current patient journey—late diagnosis, 97% ending up on dialysis, then possibly getting a transplant over the next 5 to 10 years—needs to change. It’s become the norm, and that’s not okay.
MG: I agree completely. What’s encouraging is that we’re finally seeing alignment around that need to “turn the aircraft carrier.” The landscape has changed dramatically since we launched the Coalition. We now have unprecedented opportunities to understand the scale of the CKD crisis, and the tools to do something about it.
We can now see kidney disease more clearly through lab data like eGFR results, and we’re learning how much cardiovascular mortality and spending is tied to kidney disease that has gone unrecognized. We have both visibility and solutions—guideline-directed therapies, better diagnostics, and preventive tools. That’s creating momentum among patients, providers, and payers to change the system.
KF: I’ve seen that shift too. When I first went to Kidney Week in 2008, everything was about dialysis. You go now, and it’s night and day. There’s real progress, but as someone who’s lived this, I’d say it’s long overdue. We just need to move faster.
MG: Absolutely. We can recognize progress and still acknowledge that it hasn’t come quickly enough.
What are some of the policy goals and key tactics in the white paper?
MG: We wanted this paper to be tactical. Instead of proposing new care models, which can take years to develop and evaluate, we focused on actions the Innovation Center can take now. We came up with 6 Innovation Center tactics that align with early CKD policy goals under the MAHA strategy.
Figure: Tactical Recommendations & CKD Policy Goals
A good example is expanding access to medical nutrition therapy (MNT). It’s been shown to slow disease progression, but right now it’s limited to certain patients and providers.3 Our recommendation is simple: make MNT available to all Medicare beneficiaries with CKD across every value-based care model.
The same logic applies to other benefit enhancements like kidney disease education, another intervention with strong evidence to support wider use. Why not give patients in any Innovation Center model the flexibility to access these types of benefits earlier in the disease process? The clinical, financial, and operational benefits are clear.
KF: For me, one of the most important themes is patient activation. The Executive Order from 2019 was about giving people choice: in their care, in dialysis modality, in clinical trials. Patient activation takes that a step further. It means giving patients the knowledge, skills, and confidence to manage their own health. To become active participants in their care.
I’ve experienced the power of that myself. When I was first diagnosed, I pushed back when my doctor referred me to a nephrologist who hadn’t managed my CKD well. I took ownership of my care and ended up getting the right treatment. That’s what patient activation looks like, and research shows it leads to better outcomes.4
MG: Exactly. We recommend incorporating existing measures like the Patient Activation Measure (PAM) into value-based models. Everyone agrees on the “what,” now we need to figure out the “how.” These kinds of tools help make activation measurable and actionable.
Figure: C4KH White Paper (View)
How can alignment across payers and systems accelerate progress?
MG: One of our biggest areas of focus was multipayer alignment. Most Innovation Center models are designed for fee-for-service Medicare, but more than half of beneficiaries are now in Medicare Advantage. That means incentives are fragmented.
If we want true system transformation, incentives across Medicare, MA, and commercial payers need to be aligned. We recommend CMMI convene payers and trade organizations to ask a simple question: What would help you do more on CKD earlier? Start there, then build a policy framework around it.
Figure: Medicare Advantage (MA) enrollment, 2006-22

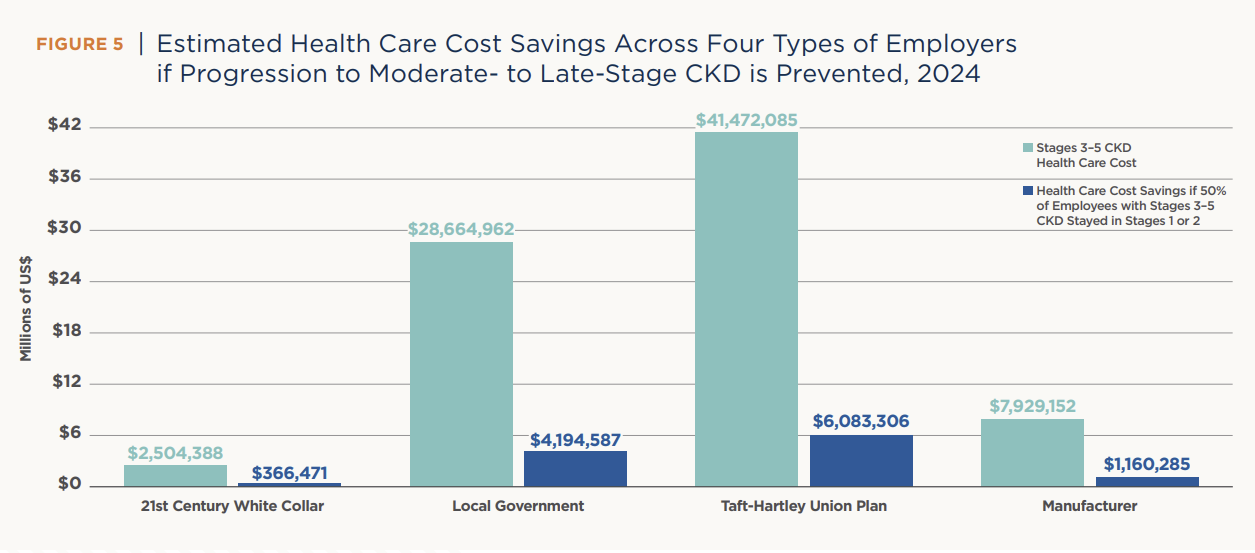
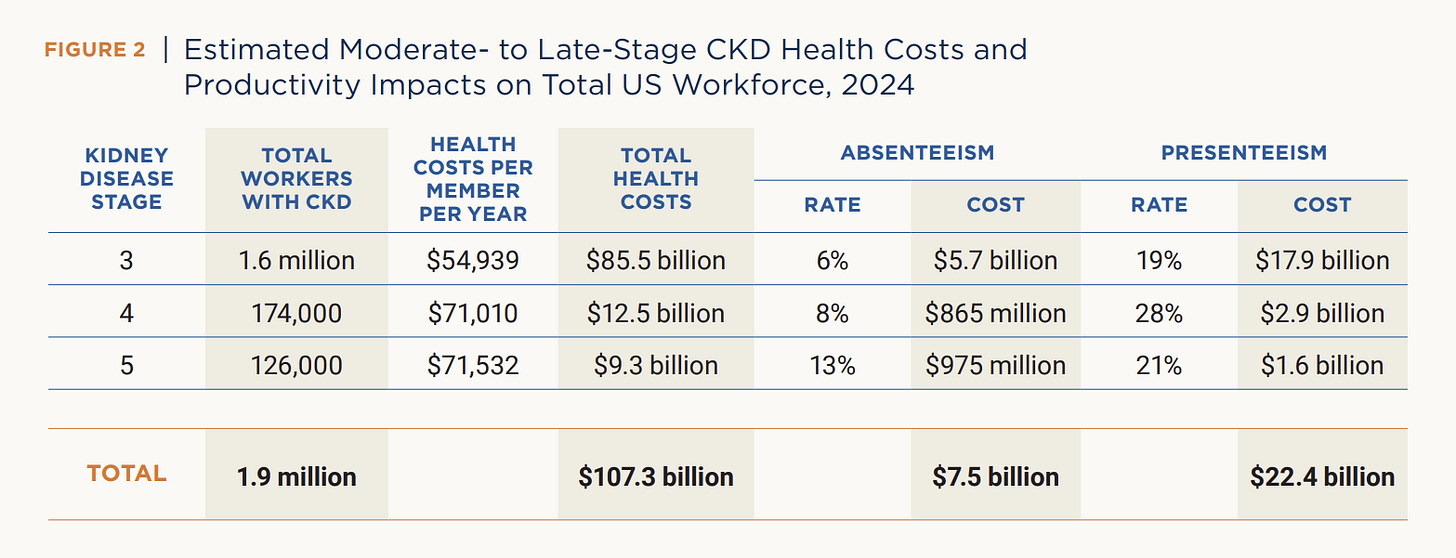
KF: And the payoff to avoiding kidney failure is enormous. The cost of end-stage kidney disease under Medicare is staggering, and that doesn’t even account for the lost productivity of people who cannot work because of their disease or dialysis.5 Prevention and early detection aren’t just moral imperatives, they’re economic ones.
MG: Policy progress is often incremental, but these tactical steps matter. Something as small as expanding nutrition therapy or education access can fundamentally change how patients experience their care.
What role does technology play in early detection and prevention?
MG: Technology and data are essential. The white paper includes recommendations around digital therapeutics and patient-facing tools that support activation and adherence.
At the end of the day, CMMI is a learning organization. Each model is evaluated on quality and savings before it becomes permanent. That gives us a chance to test what actually motivates patients and drives behavior change. We have to understand how different populations engage with technology: what works, what doesn’t, and how tools can be better integrated into care.
TF: I think that’s a key point for any innovators listening, understanding how policy shapes downstream adoption. Even if your tool works clinically, it may not reach patients or clinicians without a clear reimbursement pathway or alignment with the current system. I learned that the hard way— awareness matters.
KF: Exactly. Technology is powerful, but activation still starts with the physician–patient relationship. When you have a doctor who listens, communicates well, and treats you with respect, it changes everything. Tools like MyChart were useful for me, but trust and good communication are what drive engagement.
MG: And clinicians need to be activated too. CMS has a big opportunity to play a convening role, bringing together clinicians, payers, and innovators to share best practices and build integrated care frameworks that work for both patients and providers.
Why are integrated care models important?
MG: Integrated care is critical because kidney disease rarely exists in isolation. Most patients also have cardiovascular or metabolic conditions, and managing those together makes far more sense than addressing them separately.
When NKF first launched CKDIntercept, we even proposed a kidney-specific ACO model back in 2016. CMS didn’t move forward with it at the time—and they were right not to. But adding more silos wasn’t the answer. The real challenge is helping primary care clinicians manage complex patients with multiple conditions, including CKD, without overwhelming them.
That’s where the cardio-kidney-metabolic (CKM) framework comes in. We know that around 90% of U.S. adults have at least one CKM risk factor, and over half have two or more. So when we think about value-based care, it makes sense to integrate these conditions under shared frameworks that reflect the reality of patient care.
Figure: Stages of CKM Syndrome
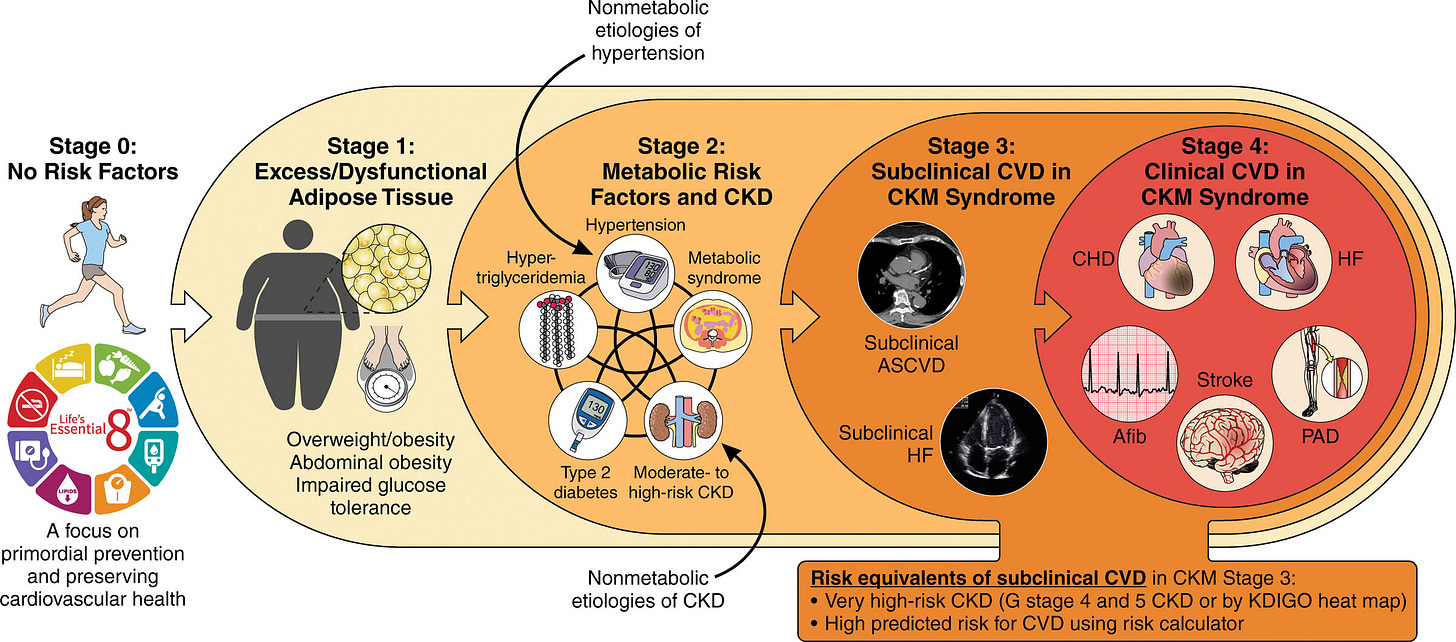
KF: I completely agree. Without a system-wide approach, too much depends on individual patient activation. After my transplant, I had to advocate on my own for cardiology and endocrinology follow-ups. That shouldn’t depend on luck or persistence—it should be built into the system. When integrated models work, they deliver coordinated care, and that benefits everyone.
MG: There’s still low-hanging fruit, too. For example, the Kidney Health Evaluation for Adults with Diabetes (KED) measure has driven more screening, but not necessarily more diagnoses. We have to close that loop: screening, diagnosing, and treating early. And care delivery should look different for different disease causes. A patient with IgA nephropathy or polycystic kidney disease will need a very different care pathway than someone with diabetes or hypertension. Policymakers need to recognize that nuance from the start.
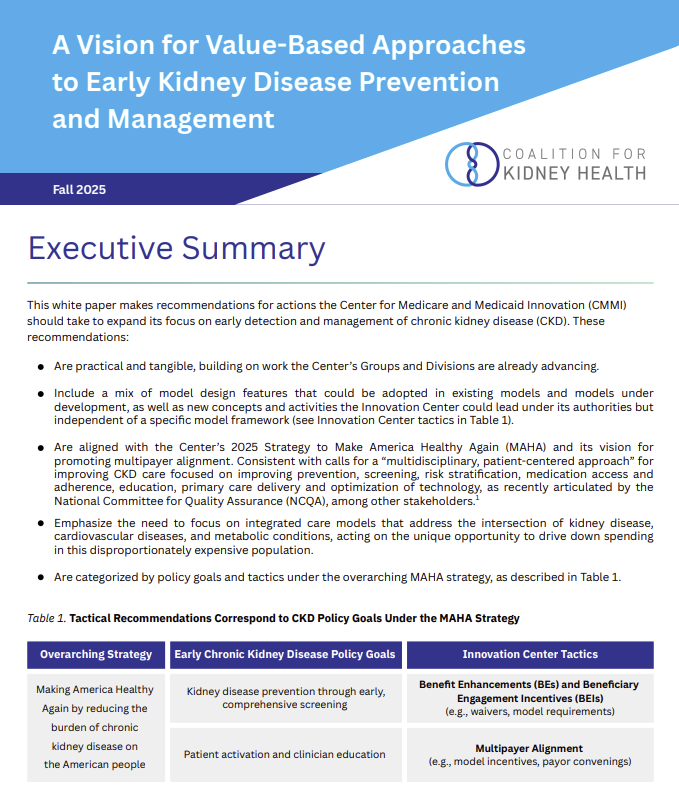
How does this align with current national health strategies like MAHA?
MG: The white paper was designed to build on the Advancing American Kidney Health Executive Order from 2019 while aligning with CMS’s current Make America Healthy Again (MAHA) strategy. The themes are remarkably consistent—prevention, patient empowerment, and competition.
When I saw MAHA’s framework, I thought, “This is tailor-made for kidney care.” Roughly 60% of kidney failure is preventable. If we can prevent even a portion of that, we’ll save lives and reduce enormous costs.
Figure: How CKD Investments Align with MAHA
Empowerment and activation are equally critical, equipping people with the tools and information they need to manage their health and make choices about their care. And when prevention isn’t possible, competition ensures patients still have real options about how and where they receive treatment.
The policy goals are clear; our job is to connect them.
KF: I’d add that it’s also an economic issue. Keeping people healthy means keeping people working. When you’re on dialysis, holding a job is incredibly difficult. I’ve been able to work for 21 years post-transplant. That’s a privilege most patients don’t get. Early detection and better management can make that the norm, not the exception. Prevention isn’t just good policy, it’s good economics.
Figure: The Cost of CKD in the U.S. Workforce
What does success look like in the next few years?
MG: We’d love to see these recommendations put to work, of course, but real success means more than that. It’s about gaining broader participation, more organizations joining this conversation and contributing their own solutions for moving kidney care upstream.
Like we said, the progress in kidney policy over the past decade has been real, but we’re just getting started. Ten years ago I was tracking 5 policy issues. Today, I’m tracking 100. If I’m tracking 500 in another ten years, I’ll count that as success (and be exhausted). It will mean the field is vibrant, the ideas are flowing, and transformation is happening on multiple fronts.
KF: For me, success is about implementation—making sure the innovations and therapies we already have actually reach patients. If we can expand access and improve uptake, especially among underserved and rural populations, we’ll start to reduce disparities instead of widening them. Everyone deserves access to the same level of innovation and care.
Who do you want to hear from next?
MG: I’d love to hear from organizations delivering value-based care—whether in kidney care, primary care, cardiology, or Medicare Advantage. Are these policy frameworks the right ones? What barriers do you face in implementing them? Policy is only as good as what happens on the ground. The real magic happens when care delivery meets policy—when clinicians and patients bring these frameworks to life.
KF: Two groups come to mind. First, patients—people living with kidney disease who want to get involved and advocate for change. We need more voices at the table. And second, innovators. If you’re building tools or solutions for kidney health, get engaged early. Understand how policy shapes the environment you’re building for. That’s how we turn innovation into impact.
Final thoughts?
KF: Everyone benefits when we focus on kidney health. We also need to support the nephrology community. Historically, the system has rewarded treating kidney failure more than preventing it, and that’s taken away opportunities for nephrologists to use their full expertise. If we design policies that reward prevention, we empower clinicians to do what they were trained to do: preserve kidney function and improve lives.
MG: I couldn’t agree more. Public policy starts with ideas, and those ideas come from people: patients, clinicians, innovators, advocates. If we understand what’s possible within the system and push creatively within those boundaries, we can change it.
To anyone listening: share your ideas, your hopes, your passion. Bring them forward. That’s how we build a better future for kidney health.
My thanks to Miriam and Kevin for joining me to share the Coalition’s work. This is a timely discussion. We recorded this a few days before heading to Kidney Week, and I’m finishing up edits as the event winds down. These topics are top of mind across the kidney ecosystem right now. No matter who you are or how you think about addressing unmet needs in this space, I’d love to hear what you think of these recommendations in the paper, and what you’d like to see policy makers do. Believe me, they’re watching the comments section. Thanks for being here.
Kidney Care Choices (KCC) Model (cms.gov)
ESRD Treatment Choices (ETC) Model (cms.gov)
CMS Innovation Center (CMMI) (cms.gov)
Advancing American Kidney Health (AAKH) (aspe.hhs.gov)
In our 2024 Expert Q&A on the future of kidney nutrition, we heard all 6 experts talk about the role of MNT in their management of patients with CKD and ESKD. It’s worth re-reading if you want a refresher on the important links between nutrition and kidney health.
Healthy Workforces, Sustainable Futures: Why Employers Should Invest in Early Kidney Care (American Kidney Fund, National Alliance of Healthcare Purchasers Coalition)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!NnOt!,w_144,h_144,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F688fc47b-7202-4a2e-b4f4-fea2b047ab1b_1500x1500.png)