I had the chance to attend the annual Digital Health New York (DHNY) Summit two weeks ago. It was a day packed with high-caliber people and discussions, the kind that felt less like casual networking and more like the early stages of a partnership. Bunny Ellerin, DHNY’s CEO, set the tone by sharing that New York now leads the nation in digital health fundraising. But the real story was the energy in the room. Between panels, investors, entrepreneurs, and health system leaders were mapping out ways to work together in real time.
That density of ideas and people made it hard not to feel optimistic. DHNY isn’t just reflecting where healthcare innovation is headed, it’s helping to set the pace.
Below are four themes that stood out across the day. I’d love to hear your take: how do you see these dynamics playing out in kidney care, cardiometabolic health, or the spaces you’re watching most closely? Let us know!
Figure: DHNY 2025 Report
1. AI Everywhere: From Empathy to Efficiency
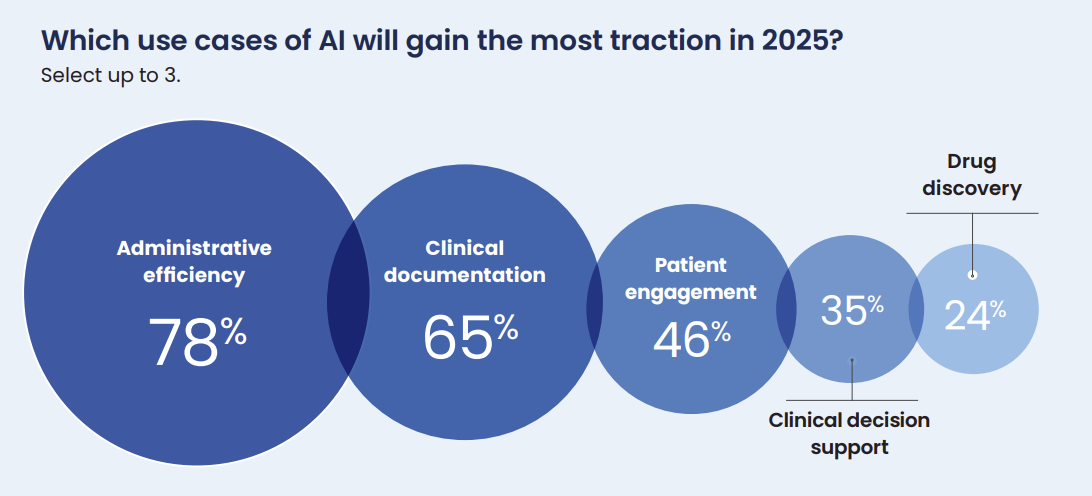
The first theme that kept surfacing, and not surprisingly, was artificial intelligence (AI). From empathy demos to workflow tools, it was everywhere.

What Happened: Nearly every conversation touched AI — whether empathy demos, physician productivity tools, payer strategies, or investor theses. Discussions explored how AI might improve mental health access, free resources for chronic care, and help address workforce shortages.
Why It Matters: AI is no longer hypothetical. Off-the-shelf models are already showing clinical reasoning and empathy. But successful adoption depends on trust, workflow fit, and patient confidence — not just technical capability.
What To Watch: Expect AI to augment (not replace) clinicians, with the next phase embedding into multi-data workflows that deliver measurable gains in outcomes and efficiency.
2. Value-Based Care, Longevity, and Home Models
Just as AI dominated the tech conversations, another set of sessions pushed toward the financing and delivery side; where value-based models, longevity, and home care are moving from aspiration to reality after decades of MA growth.
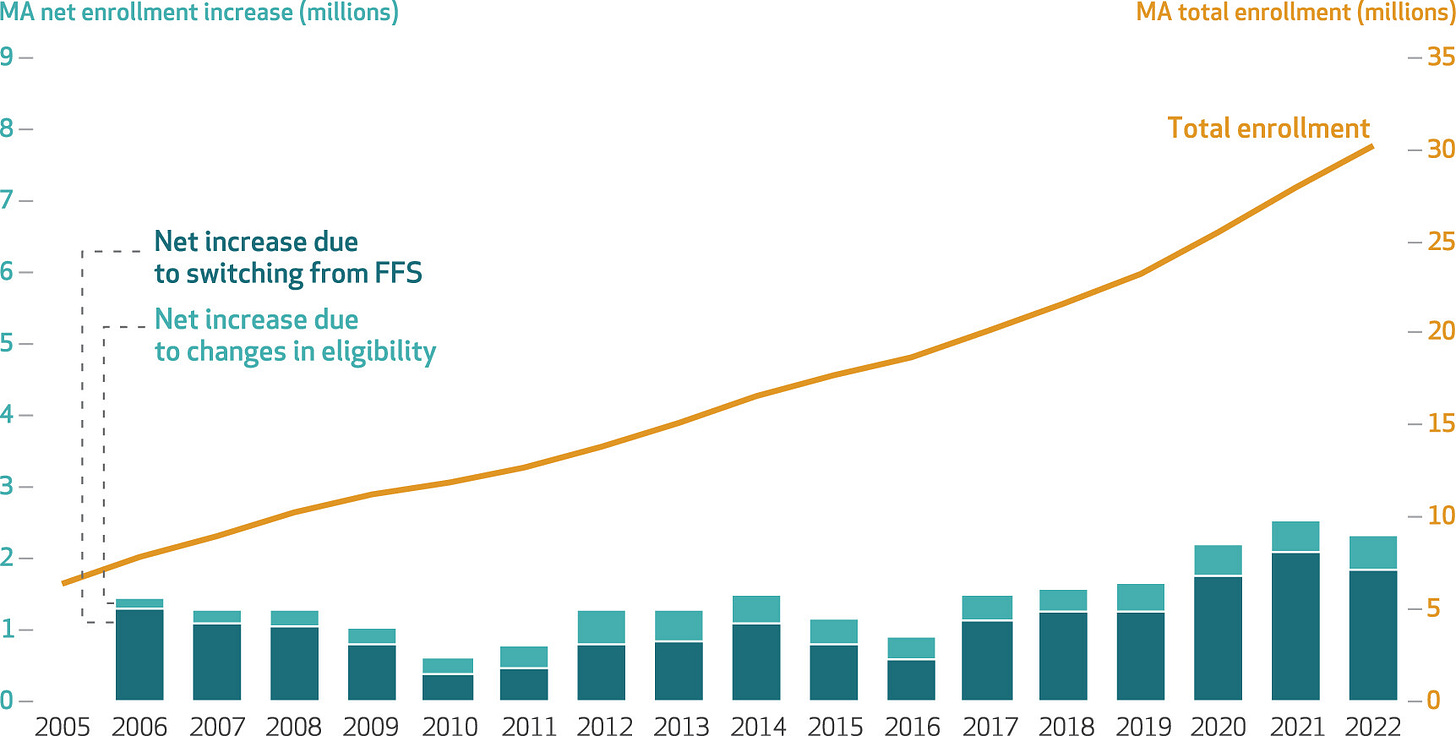
What Happened: Panels on longevity and home-based care reflected how value-based models are maturing. Longevity is shifting from a wellness trend to a systemic priority, while home care is emerging as a cost-saving imperative — though still hard to deliver consistently without regulatory and financing support.
Why It Matters: If not integrated into mainstream financing, longevity risks staying fragmented. And as Medicare Advantage grows, payers can no longer avoid home-based and end-of-life care.
What To Watch: We’ll see convergence: consumer wellness, digital health, and payer models aligning around outcomes and ROI. Longevity will increasingly be measured not in years lived, but in healthy years gained.
3. Clinician Strain and Systemic Sustainability
But all of these models depend on clinicians who can actually keep up. That brought the focus to another throughline: the unsustainable strain on physicians and the tools being designed to help them.
What Happened: Breakout sessions underscored the toll on clinicians: burnout, context-switching, documentation burdens, and the doubling pace of medical knowledge. Solutions ranged from AI scribes to secure dialers and AI search tools.
Why It Matters: Burnout and knowledge gaps aren’t just workforce challenges — they directly affect safety and cost. The system’s knowledge burden is unsustainable without change.
What To Watch: AI assistants and point-of-care education will become baseline tools. CME and pharma education will need to adapt to more responsive, digital formats.
4. Capital Flows and New York’s Rise
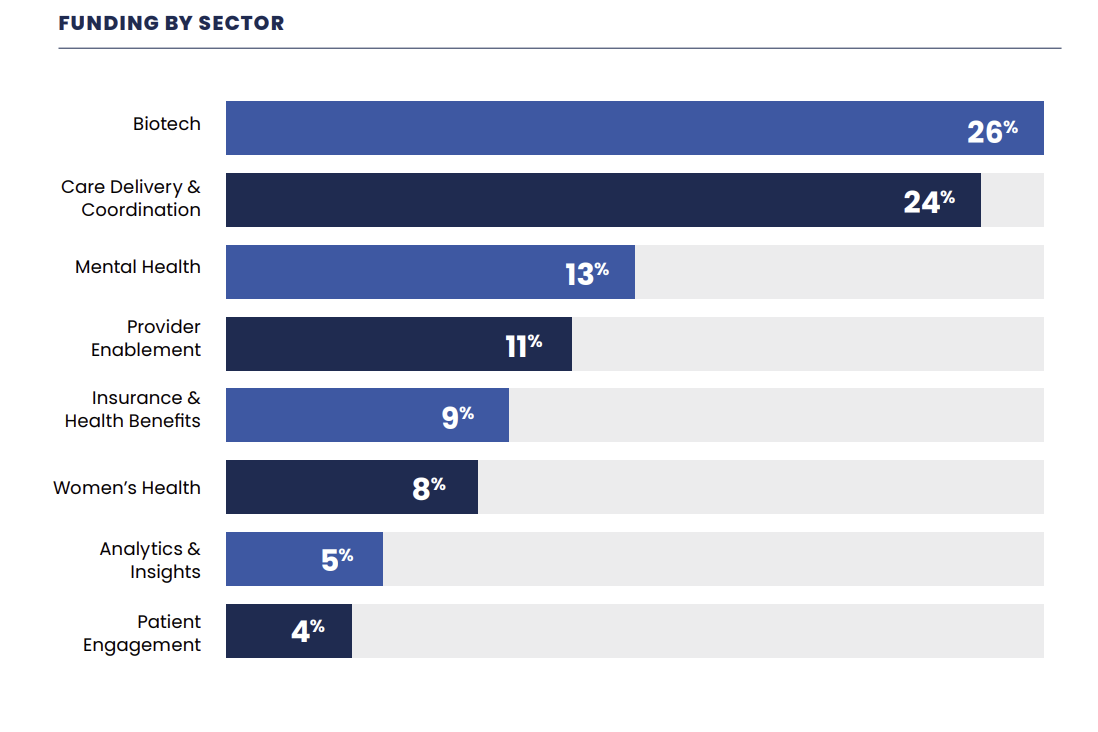
Of course, none of this takes off without capital. The investor discussions, and New York’s growing role as a health hub, underscored how money is shaping which ideas scale (and which stall).
What Happened: From Bunny Ellerin’s opening to investor insights, New York’s rise as a digital health hub was clear. Strategic investors like CVS and Lilly are bridging corporate assets with startups, while valuations are bifurcated: top performers draw oversubscribed rounds, others face punitive structures.
Why It Matters: Investor discipline is separating durable companies from opportunistic rebrands. Clean structures dominate top deals, while hype alone no longer passes.
What To Watch: New York will continue to attract talent, capital, and partnerships — rivaling Boston and the Bay Area. DHNY itself is becoming a convener of record for leaders shaping healthcare’s trajectory.
Closing Reflection
And while the summit was filled with forward-looking models, AI, and capital trends, one of the most grounding moments came from public health. I think it’s an important reminder that innovation is always layered on top of everyday systems that keep us safe.
That memorable moment for me was hearing Dr. Michelle Morse, New York City’s Acting Health Commissioner, describe the everyday work of keeping 8 million people safe. From AI models scanning thousands of data points for outbreaks to field teams engaging directly with communities, she reminded us how much of public health is both high-tech and deeply human.1
Walking away, I felt that DHNY captured the urgency and optimism of healthcare in motion. The conversations and commitments sparked here will ripple well beyond New York.
I’d love to hear your thoughts. Which of these themes feels most urgent in your world? Where do you see the biggest gap between promise and practice? Thank you for being here and let us know if you’ll be at Kidney Week!
New York Introduces Legislation to Regulate Use of Artificial Intelligence in Mental Health Care (hooperlundy.com)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)