Most founders start with a business plan. Collins Oghor started with a promise—to reimagine the care he first encountered as an 11-year-old visiting his aunt’s dialysis center in Nigeria. That promise has taken him from McGill to the UN, McKinsey, Harvard, and now Miami, where he leads Kaüna—a new model that combines practice ownership, dialysis operations, and custom-built technology to deliver value-based kidney care from the inside out.
In this conversation, Collins shares the journey behind Kaüna, what he’s learning from owning the problem firsthand, and why he’s betting on a provider-led movement to change the status quo.
In this interview, we discuss:
Collins’ journey from Nigeria to Canada, Cambridge, and Miami
Why Kaüna combines care delivery with in-house tech development
A day in the life running a nephrology practice and dialysis center
How bottom-up technology design supports value-based care
“Early” lessons after five years on front lines of kidney care
The vision for 20 centers and 200 staff in three years
Finding mission-aligned, early career nephrologists
I’ve known Collins and followed his work for about four years. This conversation was a long time coming, and I know he’s just getting started. I think you’ll enjoy this one—and I’d love to hear what questions you have for him. And if you know any early-career nephrologists or fellows looking to chart a different course in kidney care, please do share this episode with them!
Q&A
Tell us about your background and how you came to build Kaüna.
Kaüna means “love” in Hausa, a language spoken in Nigeria where I grew up. My connection to kidney care started early—when I was 11 or 12, my aunt, who I was very close to, developed end-stage renal disease. I often went with her to dialysis. One day, I told her I wanted to build a hospital like the one we were in. She believed I could, which left a lasting impression. Sadly, she passed away a few months later, but that moment sparked my drive to become both a doctor and an entrepreneur.
I moved to Canada at 17, completed pre-med, and was accepted into McGill University’s joint MD/MBA program. After graduating, I joined the UN in Geneva to work on a tuberculosis diagnostics project, then returned to start internal medicine residency—but was recruited by McKinsey & Company to work in their public and social sector practice on global health projects.
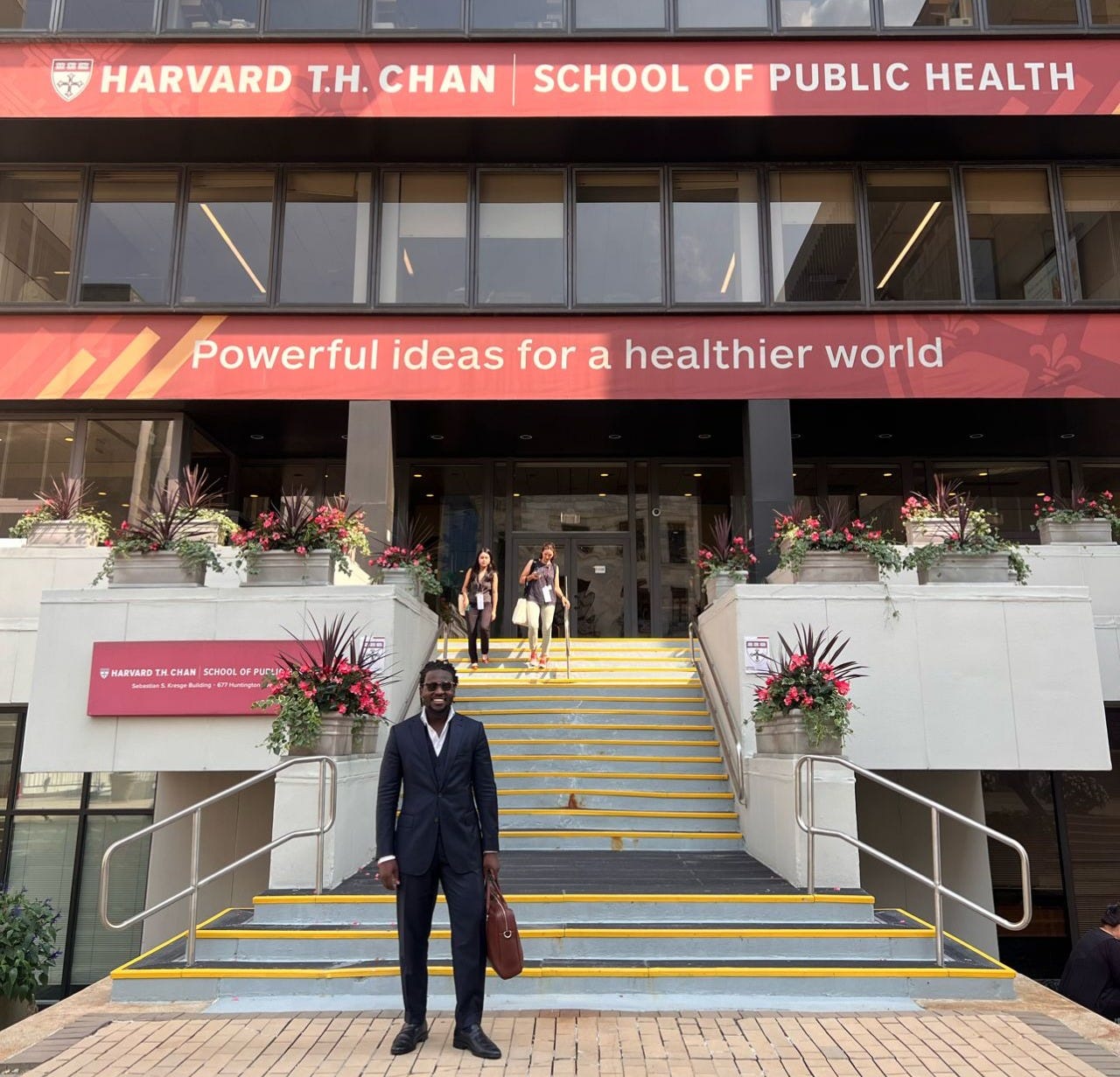
Wherever I went, kidney disease kept coming up. Around 2019–2020, with the launch of the Advancing American Kidney Health Initiative, I saw an opportunity. Nephrologists in the U.S. were about to face a new paradigm of care and would need support to make the transition. Initially, I focused on chronic care management and care coordination software. But I realized I needed deeper grounding in U.S. public health and healthcare administration, so I completed a Master of Public Health in Health Management at Harvard, focusing my program on value-based kidney care delivery.
The concept for Kaüna was born there. Today, our mission is to reimagine kidney care, and that work has brought me to Miami to start this journey.
What is the vision for Kaüna?
We are re-imagining kidney care from the ground up.
Our mission is intentionally broad—we’re not claiming to have all the answers. Instead, we ask “why” about every aspect of kidney care, aiming for transformation without discarding what already works.
I started with care coordination technology, but quickly realized practices face immense operational and regulatory pressure. To truly make change, you have to work from the inside. So we decided to acquire and operate independent nephrology practices, dialysis centers, and eventually vascular access centers, while building the technology to run them more efficiently and deliver value-based care.
We recently completed our first acquisition in South Florida. Our goal is to build a network of centers and run them differently—more efficiently, with technology designed specifically for this environment.
What does a typical day in the practice look like?
We went all in—acquiring a practice, dialysis center, peritoneal dialysis unit, and the real estate. I’m often at the center by 5 a.m. to welcome patients and staff. Seeing the early-morning challenges patients face—transport delays, long waits—has been eye-opening.
The practice side starts later in the morning, with our nephrologist seeing 25–30 patients a day. Medical assistants juggle scheduling, referrals, and reminders. Our social worker handles insurance issues, social needs, and patient support.
Midday, I meet with our five-person development team to translate the day’s operational pain points into product improvements—reducing unnecessary emails, faxes, and spreadsheets. Throughout the day, I’m also recruiting nephrologists, meeting investors, and connecting with patients during dialysis changeovers.
It’s busy, but energizing.
How does the technology fit into Kaüna’s model?
Running a center requires more than just an EMR—you need systems for finance and operations, chronic care coordination, patient engagement, HR, marketing, and more. Most clinics rely almost entirely on their EMR, with everything else handled manually via paper, fax, email, or Excel.
We’re building a modular platform that covers all these needs, designed to be open so third-party apps can integrate. It’s scalable—adding new clinics or staff has negligible marginal cost—and AI is built into workflows rather than as a separate tool. While it’s kidney-focused now, many modules could work in other specialties.
We use our own platform daily, refining it based on real-world use. The long-term plan is to make it available to like-minded centers so they can avoid juggling dozens of disconnected vendors.
You’ve said your approach to value-based care is “bottom-up.” What do you mean?
Most companies bring technology or services to a practice and try to make them fit. We start with the practice, build solutions for our own problems, and let the technology evolve from there. It’s about owning the problem and designing from the ground up.
This approach gives us skin in the game, keeps us focused on long-term results, and ensures the tech reflects the realities of day-to-day care delivery. Over time, owning the operational data—not just patient data—will also give us a strategic advantage.
We will use those learnings to challenge the status quo to think and operate differently.
What have been the biggest lessons so far?
First, everything is harder than expected. Second, dialysis truly delivers daily miracles—saving hundreds of thousands of lives nationwide—yet suffers from a negative public image. We need to change that narrative.
I’ve also been reminded that much of our industry discussion overlooks the patient experience—like the hours patients spend in transit each week. And finally, there’s a tendency to accept “that’s just the way it is.” I want to challenge that mindset and build a team that’s energized about rethinking what’s possible.
Tell us about the team you’re building.
We want a provider-led movement, starting with nephrologists who think differently and want to help shape a new model. I focus on creating roles where they get what they need to be fulfilled professionally and personally.
We’re also expanding our tech team, bringing in more AI expertise, and adding allied professionals like NPs and PAs to increase capacity. Our staff is about 30 now; we expect to grow to around 200 in three years.
How are you finding people who resonate with your vision?
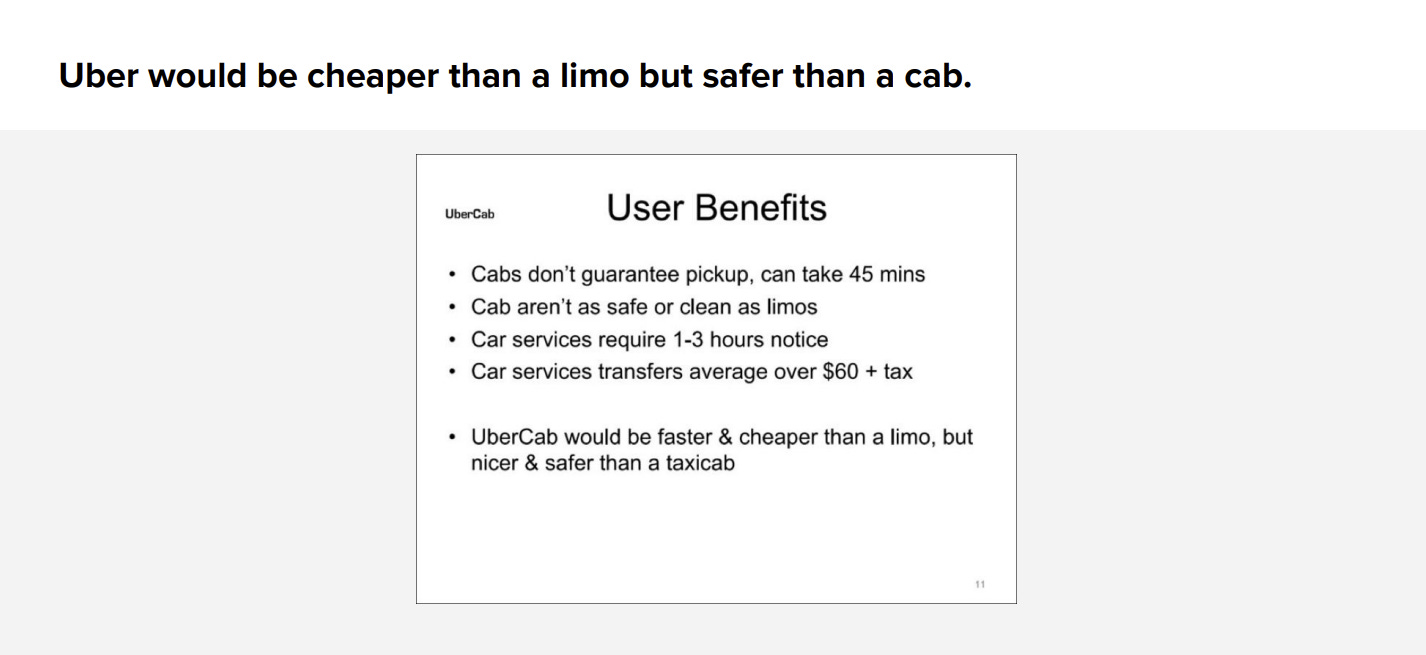
Reactions range from “genius” to “crazy”—I’m no genius, and probably somewhere in between. Early-career nephrologists, in particular, are open to disruption and new models. They’ve seen examples from other industries like Airbnb and Uber.1 Many have also seen what previous generations endured and want a different path.
Right now, outreach is very direct—calls, in-person visits—but we’re starting to build brand messaging. I think growth will come organically, with good experiences spreading by word of mouth.
What does growth look like from here?
Our immediate focus is South Florida, but we’re exploring opportunities in Georgia and Texas. When I say 20 centers, I mean combinations of practices, dialysis units, home programs, and vascular access centers—some sites will have all three.
Where do you expect your growth to happen?
Our immediate focus is South Florida, but we’re exploring opportunities in Georgia and Texas. When I say 20 centers, I mean combinations of practices, dialysis units, home programs, and vascular access centers—some sites will have all three.
Where do you hope Kaüna will be in 10 years?
I believe we’ll evolve into something valued not just as a kidney care company, but as a technology-enabled care platform—giving us the scale and resources to compete with larger players while influencing the standard of care.
If we succeed, others will feel competitive pressure to improve how they treat patients and operate their centers. We could be IPO-ready within a decade if we stay true to the mission.
Who do you want to hear from?
Early-career nephrologists who want an alternative to the status quo. Experienced clinicians—the “OGs”—who’ve seen the industry’s challenges and can share lessons learned. And most importantly, patients. Being in the center six days a week gives me constant reminders of the realities they face, and their insights are invaluable.
My thanks to Dr. Oghor for joining us and sharing his story. For more on Kaüna’s care model and growth plans, take a look at their website or reach out to Collins at collins@kauna.co. For more on what effect CMS’ recent policy changes will have on nephrology practices and where things are headed, read Kaüna’s recent white paper. Want to hear more from Collins? Catch his recent company presentation here and connect with him on LinkedIn.
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)