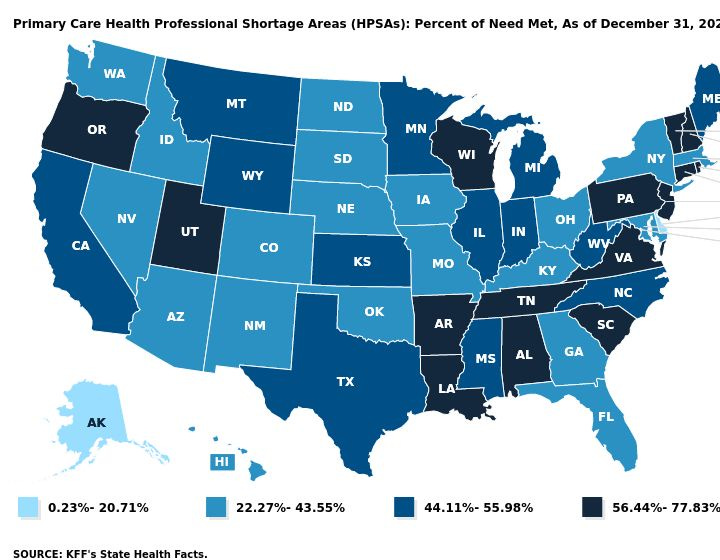
It’s long understood that primary care is the front door to kidney health — but for too many patients, that door remains closed. More than 100 million Americans live in primary care shortage areas, and in states where demand far outpaces supply, the impact shows up in fewer screenings, delayed diagnoses, and missed chances to slow chronic conditions like CKD before they progress.1
That’s where ChenMed’s model comes in. By equipping primary care physicians with tools, support, and a dedicated kidney care team, they’re reshaping what kidney care looks like in underserved communities. At the center are Chen K nurses — former dialysis nurses who educate late-stage patients, guide them through dialysis and transplant decisions, and bridge gaps between nephrology and primary care. The result: earlier intervention, smoother transitions, and more patients starting treatment with options and confidence rather than in crisis.
In this conversation, I’m joined by Dr. Virginia Irwin-Scott, ChenMed’s National Director of Kidney Care, and Jess Bean, a Chen K nurse in St. Louis. Together, they share what this model looks like on the ground: from tackling food deserts and transportation barriers to building trust in communities where healthcare has often fallen short.
In this interview, we discuss:
How ChenMed’s primary care–led model tackles CKD and ESKD in high-risk communities
The role of Chen K nurses in guiding patients through late-stage CKD and dialysis starts
Stories from the field: food deserts, transportation barriers, and building trust one patient at a time
Why strong PCP–nephrology partnerships are critical to better outcomes
Lessons for health systems: investing in navigators and care coordinators pays off
A patient-first mindset: honoring goals, whether it’s transplant, PD, or choosing no dialysis
I’ve been learning from Virginia and Jess for a while now, and this conversation brings their work to life in such a powerful way. I think you’ll find it both eye-opening and inspiring. As always, I’d love to hear your thoughts and questions — and if you know colleagues working in primary care, nursing, or kidney care navigation, please share this episode with them. These are exactly the conversations that can spark new ideas and help move the field forward.
Q&A
Can you walk us through the ChenMed model?
Virginia: ChenMed is a primary care organization serving Medicare Advantage patients, primarily in high-risk communities. Our PCP panels are small—about 350–400 patients—allowing for frequent visits, weekend teams, after-hours calls, and even outpatient ICU monitoring. Because we own the total cost of care, every hospitalization, dialysis visit, or specialist appointment comes out of our budget. That pushes us to focus on prevention, reducing admissions, and improving outcomes.
How does the “total cost of care” model shape your approach to managing CKD and ESKD?
Virginia: We go into areas where care is needed most—Miami, South DeKalb, St. Louis, Memphis, Chicago, Houston. Specialists aren’t always accessible, so we bring nephrology, cardiology, pharmacy, radiology, and other services in-house.2 This helps PCPs feel more comfortable managing complex patients while knowing they have support. It also reduces barriers for patients, many of whom live on fixed incomes and struggle with expensive copays or transportation.
What makes the difference is that the primary care physician doesn’t feel alone — they know they can lean on us for specialty-level guidance while still quarterbacking the patient’s overall health.
What unique geographic and social factors affect your population and shape your care model?
Virginia: Visiting our clinics opened my eyes to food deserts. You see fast food on every corner, but few full-service grocery stores. That reality shapes what’s possible in managing CKD. Jess sees this firsthand in St. Louis.
Jess: Right. In St. Louis, patients often rely on corner stores for meals—cheap, fried, microwave-ready foods with little fresh produce. And the landscape tells the story: you can drive through certain neighborhoods and on every corner there’s a church, a liquor store, and a dialysis clinic, but not much else. Grocery stores are closing, and the ones that remain are far from our patients. Many are elderly, don’t drive, and depend on family or unreliable public transport.
So for something as simple as food, patients are left with what’s in the neighborhood market. I’ve walked through these stores myself to see what’s actually on the shelves and then worked with patients to figure out what substitutions are realistic. It’s not about overhauling someone’s diet completely — it’s about meeting them where they are and helping them make the best choices with what’s actually available.
The ChenMed Network
Trust seems especially important in these communities. How do you build it?
Jess: Many of our patients, especially minorities, come in skeptical. Some have never had a PCP before, only ER visits. When we tell them they have kidney disease, the first reaction is often disbelief. Building trust takes time—sharing personal stories, showing lab results, relating to them as family. I tell patients, “I’m going to talk to you like I would my grandfather, who also had kidney disease and went through this.” Once that bond is built, they’re more open to education and care.
Virginia: In Memphis, one of our Chen K nurses is also a pastor’s wife. Patients trust her instantly because of that community tie. She’ll pray with them, explain things in plain language, and bridge what the PCP is saying. That kind of trust is powerful. It takes what could be a scary diagnosis and turns it into a shared journey where the patient feels seen, respected, and supported.
Let’s talk about the Chen K program. Where does kidney care navigation fit into your model?
Virginia: We think in two buckets: early CKD (Stage 3+) and advanced CKD (Stage 4–5). For early disease, we use AI and care pathways to help PCPs detect kidney problems sooner—sometimes when GFR is still 80 but proteinuria is present. For later stages, Chen K nurses—experienced dialysis nurses—step in. They educate patients, coordinate with nephrologists and surgeons, and make sure starts are “optimal.” That means no more surprise dialysis in the ER. Instead, patients transition smoothly into treatment, often with PD if possible. The goal is to eliminate the fear that comes from equating dialysis with hospitalization, and instead reframe it as a planned step in a long-term care journey.
Jess, what does a day in the life of a Chen K nurse look like?
Jess: Every day is different. With ESRD patients, we’re monitoring transportation, reviewing labs, double-checking medication reconciliation, and helping clinics with discharge planning. With CKD patients, it’s more about education—catching trends like a declining GFR, adjusting diet guidance, working with Dr. Virginia on med optimization.
We’re advocates too. If a 90-year-old tells me they don’t want dialysis, I fight for their choice, even if family pressures them otherwise. At the core, I tell patients, “Whatever your goal is, I’ll fight for it with you.”
Managing this population isn’t just medicine — it’s social work, education, logistics, and sometimes cheerleading. We’ve been called firefighters, babysitters, and bulldogs, and all of it’s true. Whether it’s arranging rides, troubleshooting fluid management, or walking a family through end-of-life decisions, the Chen K nurse becomes the steady presence that ties everything together.
How do you bridge nephrology and primary care?
Virginia: Nephrologists can’t replace PCPs. Our role is to support them—reviewing charts, answering questions, making recommendations. Often, PCPs can manage the patient with our guidance, and patients appreciate knowing a nephrologist is watching in the background.
That partnership is how we improve outcomes across such a large, complex population. And sometimes, that background review uncovers critical findings, like renal masses or early heart failure, that we can act on quickly before they spiral into crisis.
Looking ahead, what do you hope to see in the next 1–2 years?
Jess: I want us to be louder advocates—going to local governments, pushing for better transportation and resources. I’d love to see what we do become the standard of care everywhere, not just in ChenMed clinics. Patients shouldn’t have to win the lottery of geography to have this level of support.
Virginia: With policy shifts like the Cures Act and Medicaid changes, I hope we capture more patients into coordinated care.3 I also hope for clearer guardrails around transplant coverage, transportation, and reimbursement so that organizations like ours can keep providing comprehensive kidney support. If primary care is the front door to kidney health, policy is the lock and key that determines whether it can stay open.
What’s one lesson you’d share with other organizations?
Virginia: Invest in dedicated people for your highest-cost population—Stage 4–5 and ESRD. Navigators and care coordinators more than pay for themselves by preventing admissions and improving outcomes.
Jess: Always keep patients at the center. The outcomes and numbers matter, but everything falls into place when you do right by the patient. Kidney disease is a lifelong journey, and no one doctor can handle it alone—it takes a whole team. And when patients feel that wraparound support, from transportation to nutrition to trust in their care team, they don’t just stay healthier, they stay engaged. That’s when the model really works.
My thanks to Dr. Virginia and Jess for sharing your story with us. For more on ChenMed’s care model or full-risk approach, take a look at their website or this recent blog post. This conversation started after my recent articles on early CKD screening and kidney care navigation. After that discussion, it became pretty clear to me that enabling proactive kidney care has a lot more to do with equipping primary care to address a wide range of individual and community-level needs than it is about simply ordering tests. In case you missed it, you might also enjoy my recent interview with Intermountain Health’s Kidney Care team on building a nurse-led navigation program within a large integrated health system. As always, thanks for being here with us!
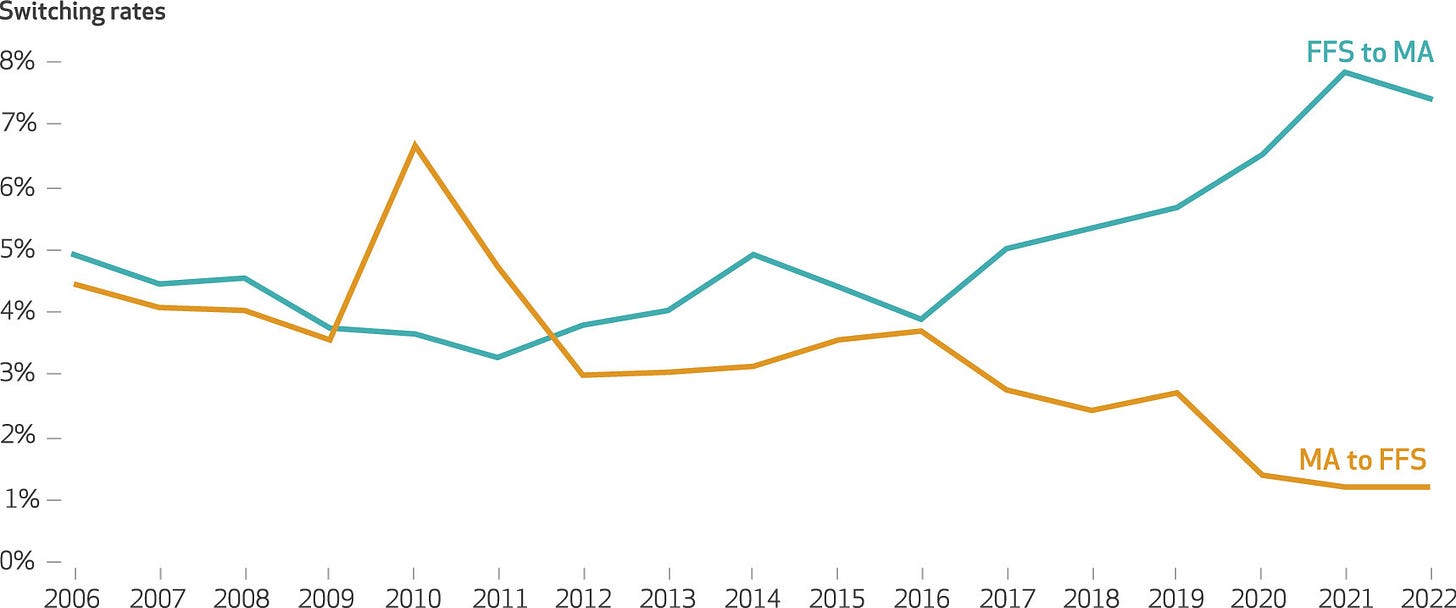
Nguyen KH, Oh EG, Meyers DJ, Kim D, Mehrotra R, Trivedi AN. Medicare Advantage Enrollment Among Beneficiaries With End-Stage Renal Disease in the First Year of the 21st Century Cures Act. JAMA. 2023;329(10):810–818. doi:10.1001/jama.2023.1426
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!IXc-!,w_40,h_40,c_fill,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F9f7142a0-6602-495d-ab65-0e4c98cc67d4_450x450.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!lBsj!,e_trim:10:white/e_trim:10:transparent/h_48,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F0e0f61bc-e3f5-4f03-9c6e-5ca5da1fa095_1848x352.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/$s_!NnOt!,w_144,h_144,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F688fc47b-7202-4a2e-b4f4-fea2b047ab1b_1500x1500.png)